Page 27 - Laparoscopic Journal - WJOLS
P. 27
WJOLS
The Future of Suprapubic Single-incision Laparoscopic Appendectomy
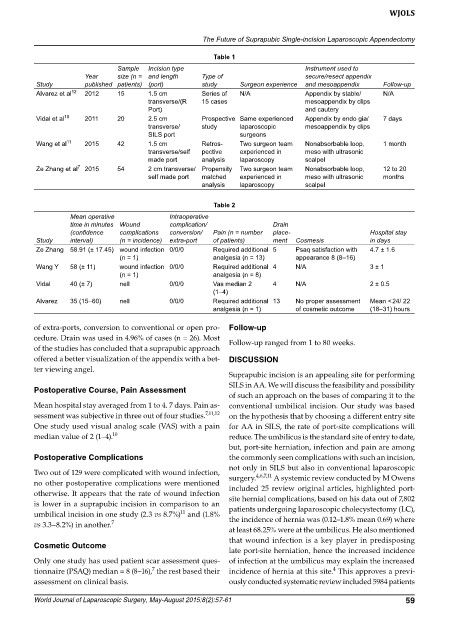
Table 1
Sample Incision type Instrument used to
year size (n = and length Type of secure/resect appendix
Study published patients) (port) study Surgeon experience and mesoappendix Follow-up
Alvarez et al 12 2012 15 1.5 cm Series of N/A Appendix by stable/ N/A
transverse/(R 15 cases mesoappendix by clips
Port) and cautery
Vidal et al 10 2011 20 2.5 cm Prospective Same experienced Appendix by endo gia/ 7 days
transverse/ study laparoscopic mesoappendix by clips
SILS port surgeons
Wang et al 11 2015 42 1.5 cm Retros- Two surgeon team Nonabsorbable loop, 1 month
transverse/self pective experienced in meso with ultrasonic
made port analysis laparoscopy scalpel
Ze Zhang et al 7 2015 54 2 cm transverse/ Propensity Two surgeon team Nonabsorbable loop, 12 to 20
self made port matched experienced in meso with ultrasonic months
analysis laparoscopy scalpel
Table 2
Mean operative Intraoperative
time in minutes Wound complication/ Drain
(confidence complications conversion/ Pain (n = number place- Hospital stay
Study interval) (n = incidence) extra-port of patients) ment Cosmesis in days
Ze Zhang 58.91 (± 17.45) wound infection 0/0/0 Required additional 5 Psaq satisfaction with 4.7 ± 1.6
(n = 1) analgesia (n = 13) appearance 8 (8–16)
Wang Y 58 (± 11) wound infection 0/0/0 Required additional 4 N/A 3 ± 1
(n = 1) analgesia (n = 8)
Vidal 40 (± 7) nell 0/0/0 Vas median 2 4 N/A 2 ± 0.5
(1–4)
Alvarez 35 (15–60) nell 0/0/0 Required additional 13 No proper assessment Mean < 24/ 22
analgesia (n = 1) of cosmetic outcome (18–31) hours
of extra-ports, conversion to conventional or open pro- Follow-up
cedure. Drain was used in 4.96% of cases (n = 26). Most Follow-up ranged from 1 to 80 weeks.
of the studies has concluded that a suprapubic approach
offered a better visualization of the appendix with a bet- diSCuSSion
ter viewing angel.
Suprapubic incision is an appealing site for performing
SILS in AA. We will discuss the feasibility and possibility
Postoperative Course, Pain Assessment
of such an approach on the bases of comparing it to the
Mean hospital stay averaged from 1 to 4. 7 days. Pain as- conventional umbilical incision. Our study was based
sessment was subjective in three out of four studies. 7,11,12 on the hypothesis that by choosing a different entry site
One study used visual analog scale (VAS) with a pain for AA in SILS, the rate of port-site complications will
median value of 2 (1–4). 10 reduce. The umbilicus is the standard site of entry to date,
but, port-site herniation, infection and pain are among
Postoperative Complications the commonly seen complications with such an incision,
not only in SILS but also in conventional laparoscopic
Two out of 129 were complicated with wound infection, surgery. 4,6,7,11 A systemic review conducted by M Owens
no other postoperative complications were mentioned included 25 review original articles, highlighted port-
otherwise. It appears that the rate of wound infection site hernial complications, based on his data out of 7,802
is lower in a suprapubic incision in comparison to an patients undergoing laparoscopic cholecystectomy (LC),
11
umbilical incision in one study (2.3 vs 8.7%) and (1.8% the incidence of hernia was (0.12–1.8% mean 0.69) where
vs 3.3–8.2%) in another. 7
at least 68.25% were at the umbilicus. He also mentioned
that wound infection is a key player in predisposing
Cosmetic outcome
late port-site herniation, hence the increased incidence
Only one study has used patient scar assessment ques- of infection at the umbilicus may explain the increased
4
7
tionnaire (PSAQ) median = 8 (8–16), the rest based their incidence of hernia at this site. This approves a previ-
assessment on clinical basis. ously conducted systematic review included 5984 patients
World Journal of Laparoscopic Surgery, May-August 2015;8(2):57-61 59