Page 24 - World Journal of Laparoscopic Surgery
P. 24
Clinical Profile and Laparoscopic Management of Hiatus Hernia
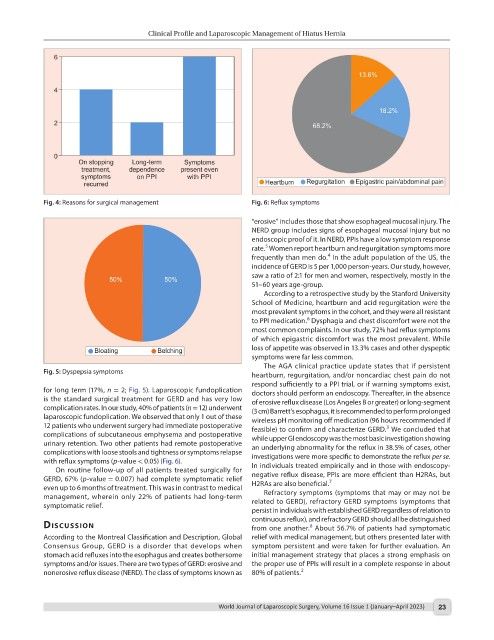
Fig. 4: Reasons for surgical management Fig. 6: Reflux symptoms
“erosive” includes those that show esophageal mucosal injury. The
NERD group includes signs of esophageal mucosal injury but no
endoscopic proof of it. In NERD, PPIs have a low symptom response
5
rate. Women report heartburn and regurgitation symptoms more
4
frequently than men do. In the adult population of the US, the
incidence of GERD is 5 per 1,000 person-years. Our study, however,
saw a ratio of 2:1 for men and women, respectively, mostly in the
51–60 years age-group.
According to a retrospective study by the Stanford University
School of Medicine, heartburn and acid regurgitation were the
most prevalent symptoms in the cohort, and they were all resistant
6
to PPI medication. Dysphagia and chest discomfort were not the
most common complaints. In our study, 72% had reflux symptoms
of which epigastric discomfort was the most prevalent. While
loss of appetite was observed in 13.3% cases and other dyspeptic
symptoms were far less common.
The AGA clinical practice update states that if persistent
Fig. 5: Dyspepsia symptoms
heartburn, regurgitation, and/or noncardiac chest pain do not
respond sufficiently to a PPI trial, or if warning symptoms exist,
for long term (17%, n = 2; Fig. 5). Laparoscopic fundoplication doctors should perform an endoscopy. Thereafter, in the absence
is the standard surgical treatment for GERD and has very low of erosive reflux disease (Los Angeles B or greater) or long-segment
complication rates. In our study, 40% of patients (n = 12) underwent (3 cm) Barrett’s esophagus, it is recommended to perform prolonged
laparoscopic fundoplication. We observed that only 1 out of these wireless pH monitoring off medication (96 hours recommended if
12 patients who underwent surgery had immediate postoperative feasible) to confirm and characterize GERD. We concluded that
3
complications of subcutaneous emphysema and postoperative while upper GI endoscopy was the most basic investigation showing
urinary retention. Two other patients had remote postoperative an underlying abnormality for the reflux in 38.5% of cases, other
complications with loose stools and tightness or symptoms relapse investigations were more specific to demonstrate the reflux per se.
with reflux symptoms (p-value < 0.05) (Fig. 6). In individuals treated empirically and in those with endoscopy-
On routine follow-up of all patients treated surgically for
GERD, 67% (p-value = 0.007) had complete symptomatic relief negative reflux disease, PPIs are more efficient than H2RAs, but
7
even up to 6 months of treatment. This was in contrast to medical H2RAs are also beneficial.
management, wherein only 22% of patients had long-term Refractory symptoms (symptoms that may or may not be
symptomatic relief. related to GERD), refractory GERD symptoms (symptoms that
persist in individuals with established GERD regardless of relation to
continuous reflux), and refractory GERD should all be distinguished
dIscussIon from one another. About 56.7% of patients had symptomatic
8
According to the Montreal Classification and Description, Global relief with medical management, but others presented later with
Consensus Group, GERD is a disorder that develops when symptom persistent and were taken for further evaluation. An
stomach acid refluxes into the esophagus and creates bothersome initial management strategy that places a strong emphasis on
symptoms and/or issues. There are two types of GERD: erosive and the proper use of PPIs will result in a complete response in about
nonerosive reflux disease (NERD). The class of symptoms known as 80% of patients. 2
World Journal of Laparoscopic Surgery, Volume 16 Issue 1 (January–April 2023) 23