Page 28 - World Journal of Laparoscopic Surgery
P. 28
Laparoscopic Cholecystectomy in Gangrenous Cholecystitis
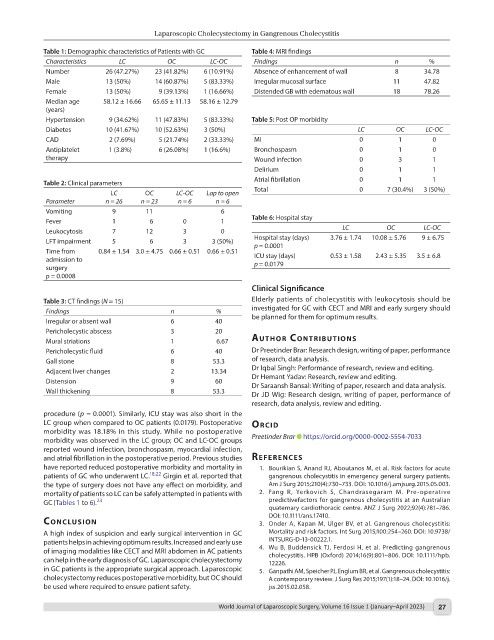
Table 1: Demographic characteristics of Patients with GC Table 4: MRI findings
Characteristics LC OC LC-OC Findings n %
Number 26 (47.27%) 23 (41.82%) 6 (10.91%) Absence of enhancement of wall 8 34.78
Male 13 (50%) 14 (60.87%) 5 (83.33%) Irregular mucosal surface 11 47.82
Female 13 (50%) 9 (39.13%) 1 (16.66%) Distended GB with edematous wall 18 78.26
Median age 58.12 ± 16.66 65.65 ± 11.13 58.16 ± 12.79
(years)
Hypertension 9 (34.62%) 11 (47.83%) 5 (83.33%) Table 5: Post OP morbidity
Diabetes 10 (41.67%) 10 (52.63%) 3 (50%) LC OC LC-OC
CAD 2 (7.69%) 5 (21.74%) 2 (33.33%) MI 0 1 0
Antiplatelet 1 (3.8%) 6 (26.08%) 1 (16.6%) Bronchospasm 0 1 0
therapy Wound infection 0 3 1
Delirium 0 1 1
Table 2: Clinical parameters Atrial fibrillation 0 1 1
LC OC LC-OC Lap to open Total 0 7 (30.4%) 3 (50%)
Parameter n = 26 n = 23 n = 6 n = 6
Vomiting 9 11 6
Fever 1 6 0 1 Table 6: Hospital stay
Leukocytosis 7 12 3 0 LC OC LC-OC
LFT impairment 5 6 3 3 (50%) Hospital stay (days) 3.76 ± 1.74 10.08 ± 5.76 9 ± 6.75
p = 0.0001
Time from 0.84 ± 1.54 3.0 ± 4.75 0.66 ± 0.51 0.66 ± 0.51 ICU stay (days) 0.53 ± 1.58 2.43 ± 5.35 3.5 ± 6.8
admission to p = 0.0179
surgery
p = 0.0008
Clinical Significance
Table 3: CT findings (N = 15) Elderly patients of cholecystitis with leukocytosis should be
Findings n % investigated for GC with CECT and MRI and early surgery should
Irregular or absent wall 6 40 be planned for them for optimum results.
Pericholecystic abscess 3 20
Mural striations 1 6.67 Author contrIbutIons
Pericholecystic fluid 6 40 Dr Preetinder Brar: Research design, writing of paper, performance
Gall stone 8 53.3 of research, data analysis.
Adjacent liver changes 2 13.34 Dr Iqbal Singh: Performance of research, review and editing.
Distension 9 60 Dr Hemant Yadav: Research, review and editing.
Dr Saraansh Bansal: Writing of paper, research and data analysis.
Wall thickening 8 53.3 Dr JD Wig: Research design, writing of paper, performance of
research, data analysis, review and editing.
procedure (p = 0.0001). Similarly, ICU stay was also short in the
LC group when compared to OC patients (0.0179). Postoperative orcId
morbidity was 18.18% in this study. While no postoperative
morbidity was observed in the LC group; OC and LC-OC groups Preetinder Brar https://orcid.org/0000-0002-5554-7033
reported wound infection, bronchospasm, myocardial infection,
and atrial fibrillation in the postoperative period. Previous studies references
have reported reduced postoperative morbidity and mortality in 1. Bourikian S, Anand RJ, Aboutanos M, et al. Risk factors for acute
patients of GC who underwent LC. 18,22 Girgin et al. reported that gangrenous cholecystitis in emergency general surgery patients.
the type of surgery does not have any effect on morbidity, and Am J Surg 2015;210(4):730–733. DOI: 10.1016/j.amjsurg.2015.05.003.
mortality of patients so LC can be safely attempted in patients with 2. Fang R, Yerkovich S, Chandrasegaram M. Pre-operative
GC(Tables 1 to 6). 23 predictivefactors for gangrenous cholecystitis at an Australian
quaternary cardiothoracic centre. ANZ J Surg 2022;92(4):781–786.
DOI: 10.1111/ans.17410.
conclusIon 3. Onder A, Kapan M, Ulger BV, et al. Gangrenous cholecystitis:
A high index of suspicion and early surgical intervention in GC Mortality and risk factors. Int Surg 2015;100:254–260. DOI: 10.9738/
patients helps in achieving optimum results. Increased and early use INTSURG-D-13-00222.1.
of imaging modalities like CECT and MRI abdomen in AC patients 4. Wu B, Buddensick TJ, Ferdosi H, et al. Predicting gangrenous
can help in the early diagnosis of GC. Laparoscopic cholecystectomy cholecystitis. HPB (Oxford) 2014;16(9):801–806. DOI: 10.1111/hpb.
12226.
in GC patients is the appropriate surgical approach. Laparoscopic 5. Ganpathi AM, Speicher PJ, Englum BR, et al. Gangrenous cholecystitis:
cholecystectomy reduces postoperative morbidity, but OC should A contemporary review. J Surg Res 2015;197(1):18–24. DOI: 10.1016/j.
be used where required to ensure patient safety. jss.2015.02.058.
World Journal of Laparoscopic Surgery, Volume 16 Issue 1 (January–April 2023) 27