Page 53 - WJOLS
P. 53
Thoracic Epidural versus Morphine Patient Controlled Analgesia After Laparoscopic Colectomy
TABLE 2: VRS pain score, TEA/ PCA adverse effects and length epidurals and without the need for intravenous “rescue” opiate
of hospital stay for patients managed with TEA or PCA following analgesia.
laparoscopic colectomy
As well as the humanitarian argument in offering optimum
TEA PCA pain relief to patients, the physiological benefits of improved
(n = 8) (n = 8) p value pain relief with TEA following open surgery include reductions
8
in the incidence of cardiac and respiratory complications and a
VRS pain score** 9
Recovery 0 (0-0) 5.3 (3.6-6.9) <0.0001¶ reduction in the duration of gastrointestinal ileus. Although
6 hours 1 (0-2.0) 5.4 (4.2-6.5) 0.001¶ these benefits have only been proven to result in improved
12 hours 0.4 (0-1.1) 4.4 (3.3-5.4) <0.0001¶ outcomes for high risk patients (ASA ≥ III) undergoing high
24 hours 1.3 (0-2.8) 5.9 (4.9-6.9) 0.002¶ risk surgery. There is evidence of similar improved outcomes
48 hours 2.8 (0.8-4.7) 4.1 (2.5-5.8) 0.218¶
with the use TEA in laparoscopic colectomy with a reduction in
6
TEA/ PCA adverse hospital stay and accelerated return of bowel function and
7
effects dietary intake. However in our study the improved pain scores
Nausea and vomiting 2 (25%) 5 (63%) of the TEA group within the first 24 hours did not translate into
Hypotension 2 (25%) 2 (25%) a reduction in length of hospital stay (5 [4-5] vs 4 [3.3-6.8]
Respiratory depression 0 0 days). This may be due to the small numbers in our study as the
Pruritis 1 (13%) 0
markedly higher mean pain scores within the PCA group (4.4-
Length hospital stay (days)* 5(4-5) 4(3.3-6.8) 0.91§ 5.9 vs. 0-1.3) would be expected to reduce respiratory function
and the patient’s ability to mobilize. Length of hospital stay is
Values are *median (interquartile range), **mean (95% CI) or number
(proportion). P values calculated using ¶Paired t-test, § Mann-Whitney also a crude measure of postoperative complications and may
U-test. cover over differences in minor complications. Also of note the
patients in our study were relatively young (73 yrs [54-77] and
61 yrs [31-68]) and fit (12 of 16 ASA I or II) which may mean as
with open surgery the major benefits in terms of improved
outcomes will be seen in high risk patients.
Adverse effects of analgesia were noted in significant
numbers of patients in both groups. Hypotension was seen in
both the TEA and PCA cohorts (2 [25%]). These figures are
consistent with previously published incidences (37-80%) of
complications due to autonomic blockade with the use of TEA. 8
There appeared to be a notably high incidence of nausea and
vomiting associated with PCA. This is unsurprising given that
this group of patients will have experienced much higher
systemic concentrations of morphine. The use of fentanyl in
the TEA infusion may also have been significant, given that it
is associated with a lower incidence of nausea and vomiting in
comparison to morphine.
Retrospective studies may be subject to bias in case
selection. We have included all the laparoscopic colectomies
performed at our hospital and excluded only those converted
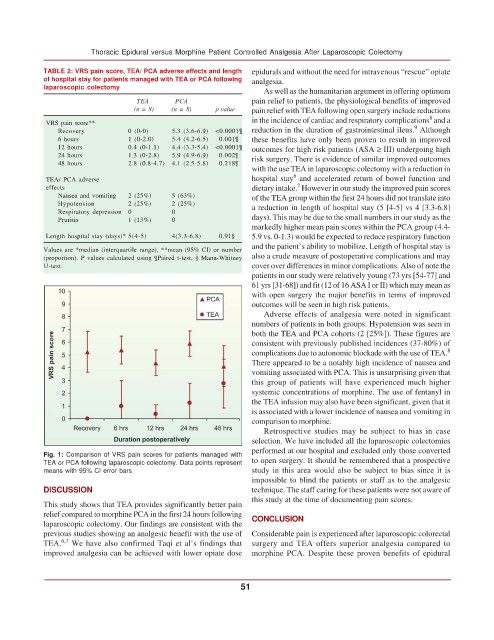
Fig. 1: Comparison of VRS pain scores for patients managed with
TEA or PCA following laparoscopic colectomy. Data points represent to open surgery. It should be remembered that a prospective
means with 95% CI error bars. study in this area would also be subject to bias since it is
impossible to blind the patients or staff as to the analgesic
DISCUSSION technique. The staff caring for these patients were not aware of
this study at the time of documenting pain scores.
This study shows that TEA provides significantly better pain
relief compared to morphine PCA in the first 24 hours following CONCLUSION
laparoscopic colectomy. Our findings are consistent with the
previous studies showing an analgesic benefit with the use of Considerable pain is experienced after laparoscopic colorectal
6,7
TEA. We have also confirmed Taqi et al’s findings that surgery and TEA offers superior analgesia compared to
improved analgesia can be achieved with lower opiate dose morphine PCA. Despite these proven benefits of epidural
51