Page 57 - WJOLS
P. 57
Laparoscopic Sugery for Rectal Carcinoma—An Experience of 20 Cases in a Government Sector Hospital
1. No incidence of port site metastasis. intracorporeal vascular control and dissection in limited space
2. Two patients with malignant melanoma reported local in pelvis, particularly in male patients. However, there are now
recurrence and 2 patients reported liver metastasis after numerous reports of successful rectal surgery by laparoscopic
approximately 1 year (one of GIST and other of Adenoca. route which prove the technical feasibility of this approach. 6,7
3. Three cancer related mortality Appealing operation early in the laparoscopic proctectomy
4. Average follow-up was 20 months (longest follow-up being was abdominoperineal resection (APR). LAPR has a number of
30 months) (Table 1). decisive advantages in comparison with other colorectal
procedures as difficult technical problem of anastomosis is
DISCUSSION obviated whereas the perineal aspect of rectum amputation
remains unchanged and it is possible to complete TME via
Open surgery was the gold standard in colorectal cancer but perineal approach. In addition, recovery of the resected
the laparoscopic surgery for colorectal cancer has gained wide specimen is unproblematic and no additional abdominal incision
acceptance over last decade. Just as laparoscopic surgery has is required. Finally, laparoscopic manipulations involve only
revolutionized the practice of biliary surgery in recent past; it is non tumor bearing segments of the bowel. 12
all set to take colorectal surgery by storm. In non-randomized comparative studies, laparoscopic and
In our series, 20 cases of rectal carcinoma were subjected open excision of rectal cancer was found to be equivalent in
to Laparoscopic Anterior Resection or Abdominoperineal achieving distal and radial negative margins. 8
Resection, the results supports use of laparoscopic technique. Adequacy of radial resection can also be measured by ability
After almost 10 years of clinical application, use of to achieve high ligation, specimen characteristics and lymph
laparoscopy for treatment of colorectal cancer is still node yield which in many recent studies have shown to be
controversial because long term outcome in malignancy is of comparable in open and laparoscopic group. 8
overwhelming importance compared with potential benefits In vast majority of reports, postoperative mortality rates
obtained in the early postoperative course and advantages in following laparoscopic rectal cancer excision were low—overall
4
cosmesis. There were serious concerns about potential mortality rate in the literature is 1.3% (Table 3). Laparoscopic
8
inadequacy of resection, possible staging inaccuracies or possi- approach did not jeopardize outcomes with probabilities of
bility that use of pneumoperitoneum altered the patterns of survival and being disease free at 5 years being as good as that
tumor dissemination. 5 for open resection. Patterns of recurrence do not appear to be
9
This is true for colon cancer and even more so far rectal different between laparoscopic and open colectomy and
cancer which is much more of challenge for laparoscopic incidence of port site recurrence in recent studies has been
surgeon because of steep learning curve it entails, need for approx. 0.1% or less. 10
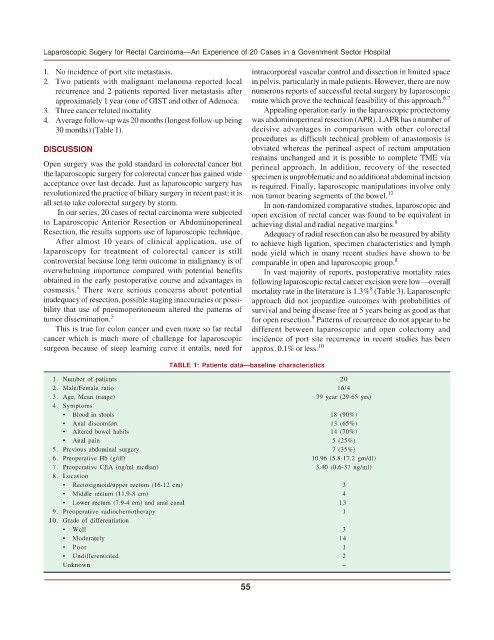
TABLE 1: Patients data—baseline characteristics
1. Number of patients 20
2. Male/Female ratio 16/4
3. Age, Mean (range) 39 year (29-65 yrs)
4. Symptoms
• Blood in stools 18 (90%)
• Anal discomfort 13 (65%)
• Altered bowel habits 14 (70%)
• Anal pain 5 (25%)
5. Previous abdominal surgery 7 (35%)
6. Preoperative Hb (g/dl) 10.96 (5.8-17.2 gm/dl)
7. Preoperative CEA (ng/ml median) 3.40 (0.6-37 ng/ml)
8. Location
• Rectosigmoid/upper rectum (16-12 cm) 3
• Middle rectum (11.9-8 cm) 4
• Lower rectum (7.9-4 cm) and anal canal 13
9. Preoperative radiochemotherapy 1
10. Grade of differentiation
• Well 3
• Moderately 14
• Poor 1
• Undifferentiated 2
Unknown –
55