Page 52 - WJOLS
P. 52
RJ Dennis, P Mills
Anesthesia and Epidural Techniques TEA or PCA, namely nausea and vomiting requiring treatment
with an antiemetic, hypotension (systolic BP < 100 mmHg)
Preoperatively patients were visited by members of the acute respiratory depression (respiratory rate < 10 breaths per minute)
pain service and received detailed oral and written information and pruritis.
on the verbal rating pain scoring scheme and the method of
postoperative analgesia that would be provided dependent on
Consultant Anaesthetic preference. No patients received pre- STATISTICS
medication. Demographic data is presented as median (interquartile range)
Patients who had TEA all had the catheters placed at the or number (proportion) and analyzed by Mann-Whitney
mid-thoracic dermatomal level T7/8 or T8/9 prior to anesthesia. U-test. Pain scores are presented as means and 95% confidence
The epidural block was established with incremental doses of intervals and analyzed by paired t tests.
0.25% L-Bupivacaine up to maximum dose of 15 ml. General
anesthesia in both the TEA and PCA groups was induced with RESULTS
propofol (2-3 mg/kg) and fentanyl (1-2 mg/kg) and muscle
relaxation achieved with rocuronium prior to intubation of the Sixteen patients were identified having undergone laparoscopic
trachea and ventilation. Anesthesia was maintained with colectomy. Eight had been managed with TEA and 8 managed
sevoflurane in an air/oxygen mixture. The PCA group received with PCA. The demographic data of these groups is summarized
morphine intraoperatively up to a maximum dose of 15 mg. Both in Table 1.
groups had intravenous paracetamol 1gm and this was
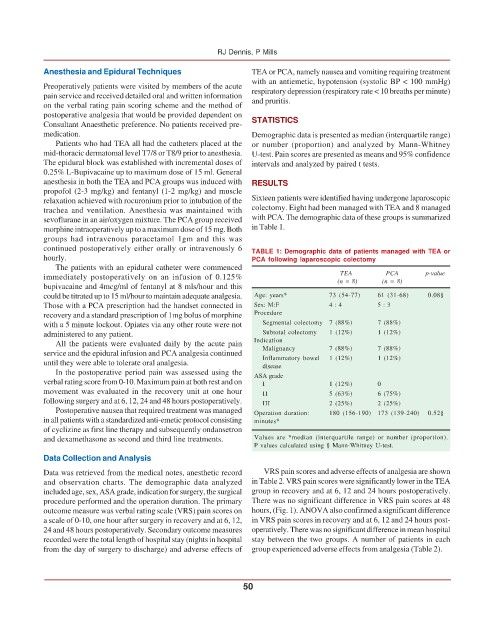
continued postoperatively either orally or intravenously 6 TABLE 1: Demographic data of patients managed with TEA or
hourly. PCA following laparoscopic colectomy
The patients with an epidural catheter were commenced
immediately postoperatively on an infusion of 0.125% TEA PCA p-value
bupivacaine and 4mcg/ml of fentanyl at 8 mls/hour and this (n = 8) (n = 8)
could be titrated up to 15 ml/hour to maintain adequate analgesia. Age: years* 73 (54-77) 61 (31-68) 0.08§
Those with a PCA prescription had the handset connected in Sex: M:F 4 : 4 5 : 3
recovery and a standard prescription of 1mg bolus of morphine Procedure
with a 5 minute lockout. Opiates via any other route were not Segmental colectomy 7 (88%) 7 (88%)
administered to any patient. Subtotal colectomy 1 (12%) 1 (12%)
All the patients were evaluated daily by the acute pain Indication
service and the epidural infusion and PCA analgesia continued Malignancy 7 (88%) 7 (88%)
until they were able to tolerate oral analgesia. Inflammatory bowel 1 (12%) 1 (12%)
disease
In the postoperative period pain was assessed using the
verbal rating score from 0-10. Maximum pain at both rest and on ASA grade 1 (12%) 0
I
movement was evaluated in the recovery unit at one hour II 5 (63%) 6 (75%)
following surgery and at 6, 12, 24 and 48 hours postoperatively. III 2 (25%) 2 (25%)
Postoperative nausea that required treatment was managed Operation duration: 180 (156-190) 173 (139-240) 0.52§
in all patients with a standardized anti-emetic protocol consisting minutes*
of cyclizine as first line therapy and subsequently ondansetron
and dexamethasone as second and third line treatments. Values are *median (interquartile range) or number (proportion).
P values calculated using § Mann-Whitney U-test.
Data Collection and Analysis
Data was retrieved from the medical notes, anesthetic record VRS pain scores and adverse effects of analgesia are shown
and observation charts. The demographic data analyzed in Table 2. VRS pain scores were significantly lower in the TEA
included age, sex, ASA grade, indication for surgery, the surgical group in recovery and at 6, 12 and 24 hours postoperatively.
procedure performed and the operation duration. The primary There was no significant difference in VRS pain scores at 48
outcome measure was verbal rating scale (VRS) pain scores on hours, (Fig. 1). ANOVA also confirmed a significant difference
a scale of 0-10, one hour after surgery in recovery and at 6, 12, in VRS pain scores in recovery and at 6, 12 and 24 hours post-
24 and 48 hours postoperatively. Secondary outcome measures operatively. There was no significant difference in mean hospital
recorded were the total length of hospital stay (nights in hospital stay between the two groups. A number of patients in each
from the day of surgery to discharge) and adverse effects of group experienced adverse effects from analgesia (Table 2).
50