Page 26 - World Journal of Laparoscopic Surgery
P. 26
Fusi Mosai, Zach M Koto
pus subgroup. The most frequent intraoperative finding complication rate was 5% and majority were from the
in this subgroup was pelvic collection. four-quadrant subgroup and the commonest complica-
The complications were divided into two major tion was pelvic collections.
categories namely intraoperative and postoperative The most common cause of morbidity was pneumo-
complications. Intraoperative complication rate was 0.5% nia. Mortality was grouped according to the subgroups,
and majority were from the four-quadrant pus subgroup which indicated high mortality rate being among the
and all were iatrogenic bowel injuries. Postoperative four-quadrant pus subgroup and significant cause was
systemic sepsis.
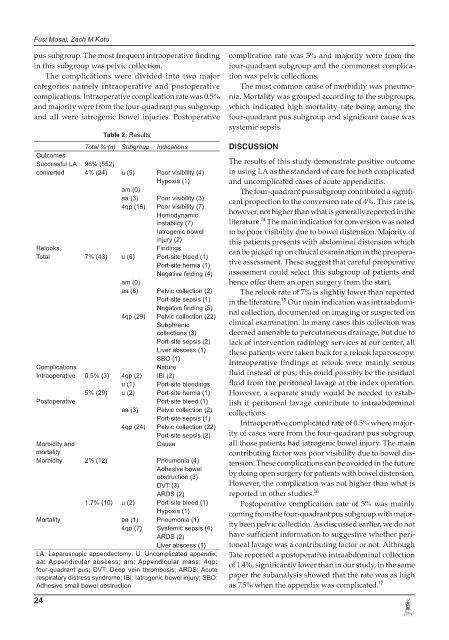
Table 2: Results
Total % (n) Subgroup Indications DISCUSSION
Outcomes
Successful LA 96% (552) The results of this study demonstrate positive outcome
converted 4% (24) u (5) Poor visibility (4) in using LA as the standard of care for both complicated
Hypoxia (1) and uncomplicated cases of acute appendicitis.
am (0) The four-quadrant pus subgroup contributed a signifi-
aa (3) Poor visibility (3) cant proportion to the conversion rate of 4%. This rate is,
4qp (16) Poor visibility (7)
Hemodynamic however, not higher than what is generally reported in the
14
instability (7) literature. The main indication for conversion was noted
Iatrogenic bowel to be poor visibility due to bowel distension. Majority of
injury (2) this patients presents with abdominal distension which
Relooks Findings can be picked up on clinical examination in the preopera-
Total 7% (43) u (6) Port-site bleed (1)
Port-site hernia (1) tive assessment. These suggest that careful preoperative
Negative finding (4) assessment could select this subgroup of patients and
am (0) hence offer them an open surgery from the start.
aa (8) Pelvic collection (2) The relook rate of 7% is slightly lower than reported
Port-site sepsis (1) in the literature. Our main indication was intraabdomi-
15
Negative finding (5)
4qp (29) Pelvic collection (22) nal collection, documented on imaging or suspected on
Subphrenic clinical examination. In many cases this collection was
collections (3) deemed amenable to percutaneous drainage, but due to
Port-site sepsis (2) lack of intervention radiology services at our center, all
Liver abscess (1) these patients were taken back for a relook laparoscopy.
SBO (1) Intraoperative findings at relook were mainly serous
Complications Nature
Intraoperative 0.5% (3) 4qp (2) IBI (2) fluid instead of pus; this could possibly be the residual
u (1) Port-site bleedings fluid from the peritoneal lavage at the index operation.
5% (29) u (2) Port-site hernia (1) However, a separate study would be needed to estab-
Postoperative Port-site bleed (1) lish if peritoneal lavage contribute to intraabdominal
aa (3) Pelvic collection (2) collections.
Port-site sepsis (1)
4qp (24) Pelvic collection (22) Intraoperative complicated rate of 0.5% where major-
Port-site sepsis (2) ity of cases were from the four-quadrant pus subgroup,
Morbidity and Cause all those patients had iatrogenic bowel injury. The main
mortality contributing factor was poor visibility due to bowel dis-
Morbidity 2% (12) Pneumonia (4) tension. These complications can be avoided in the future
Adhesive bowel
obstruction (3) by doing open surgery for patients with bowel distension.
DVT (3) However, the complication was not higher than what is
ARDS (2) reported in other studies. 16
1.7% (10) u (2) Port-site bleed (1) Postoperative complication rate of 5% was mainly
Hypoxia (1) coming from the four-quadrant pus subgroup with major-
Mortality aa (1) Pneumonia (1) ity been pelvic collection. As discussed earlier, we do not
4qp (7) Systemic sepsis (4)
ARDS (2) have sufficient information to suggestive whether peri-
Liver abscess (1) toneal lavage was a contributing factor or not. Although
LA: Laparoscopic appendectomy; U: Uncomplicated appendix; Tate reported a postoperative intraabdominal collection
aa: Appendicular abscess; am: Appendicular mass; 4qp: of 1.4%, significantly lower than in our study, in the same
four-quadrant pus; DVT: Deep vein thrombosis; ARDS: Acute
respiratory distress syndrome; IBI: Iatrogenic bowel injury; SBO: paper the subanalysis showed that the rate was as high
Adhesive small bowel obstruction as 7.5% when the appendix was complicated. 17
24