Page 22 - World Journal of Laparoscopic Surgery
P. 22
Mohammed Hamdy Abdelhady, Asaad F Salama
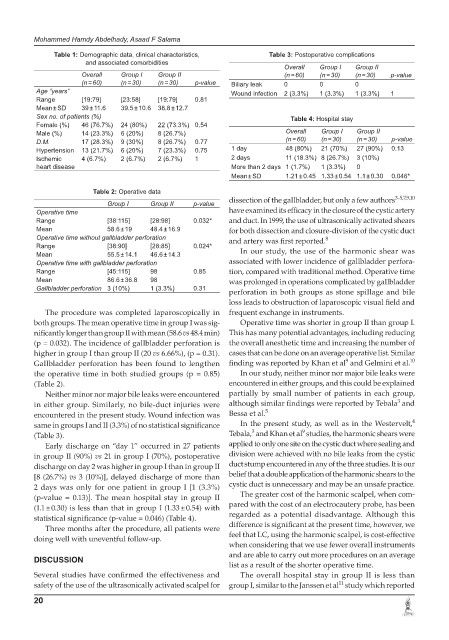
Table 1: Demographic data, clinical characteristics, Table 3: Postoperative complications
and associated comorbidities
Overall Group I Group II
Overall Group I Group II (n = 60) (n = 30) (n = 30) p-value
(n = 60) (n = 30) (n = 30) p-value Biliary leak 0 0 0
Age “years” Wound infection 2 (3.3%) 1 (3.3%) 1 (3.3%) 1
Range [19:79] [23:58] [19:79] 0.81
Mean ± SD 39 ± 11.6 39.5 ± 10.6 38.8 ± 12.7
Sex no. of patients (%) Table 4: Hospital stay
Female (%) 46 (76.7%) 24 (80%) 22 (73.3%) 0.54
Male (%) 14 (23.3%) 6 (20%) 8 (26.7%) Overall Group I Group II
D.M. 17 (28.3%) 9 (30%) 8 (26.7%) 0.77 (n = 60) (n = 30) (n = 30) p-value
Hypertension 13 (21.7%) 6 (20%) 7 (23.3%) 0.75 1 day 48 (80%) 21 (70%) 27 (90%) 0.13
Ischemic 4 (6.7%) 2 (6.7%) 2 (6.7%) 1 2 days 11 (18.3%) 8 (26.7%) 3 (10%)
heart disease More than 2 days 1 (1.7%) 1 (3.3%) 0
Mean ± SD 1.21 ± 0.45 1.33 ± 0.54 1.1 ± 0.30 0.046*
Table 2: Operative data
dissection of the gallbladder, but only a few authors 3-5,7,9,10
Group I Group II p-value
Operative time have examined its efficacy in the closure of the cystic artery
Range [38:115] [28:98] 0.032* and duct. In 1999, the use of ultrasonically activated shears
Mean 58.6 ± 19 48.4 ± 16.9 for both dissection and closure-division of the cystic duct
Operative time without gallbladder perforation and artery was first reported. 8
Range [38:90] [28:85] 0.024*
Mean 55.5 ± 14.1 46.6 ± 14.3 In our study, the use of the harmonic shear was
Operative time with gallbladder perforation associated with lower incidence of gallbladder perfora-
Range [45:115] 98 0.85 tion, compared with traditional method. Operative time
Mean 86.6 ± 36.8 98 was prolonged in operations complicated by gallbladder
Gallbladder perforation 3 (10%) 1 (3.3%) 0.31
perforation in both groups as stone spillage and bile
loss leads to obstruction of laparoscopic visual field and
The procedure was completed laparoscopically in frequent exchange in instruments.
both groups. The mean operative time in group I was sig- Operative time was shorter in group II than group I.
nificantly longer than group II with mean (58.6 vs 48.4 min) This has many potential advantages, including reducing
(p = 0.032). The incidence of gallbladder perforation is the overall anesthetic time and increasing the number of
higher in group I than group II (20 vs 6.66%), (p = 0.31). cases that can be done on an average operative list. Similar
9
Gallbladder perforation has been found to lengthen finding was reported by Khan et al and Gelmini et al. 10
the operative time in both studied groups (p = 0.85) In our study, neither minor nor major bile leaks were
(Table 2). encountered in either groups, and this could be explained
Neither minor nor major bile leaks were encountered partially by small number of patients in each group,
3
in either group. Similarly, no bile-duct injuries were although similar findings were reported by Tebala and
encountered in the present study. Wound infection was Bessa et al. 5
4
same in groups I and II (3.3%) of no statistical significance In the present study, as well as in the Westervelt,
9
3
(Table 3). Tebala, and Khan et al studies, the harmonic shears were
Early discharge on “day 1” occurred in 27 patients applied to only one site on the cystic duct where sealing and
in group II (90%) vs 21 in group I (70%), postoperative division were achieved with no bile leaks from the cystic
discharge on day 2 was higher in group I than in group II duct stump encountered in any of the three studies. It is our
[8 (26.7%) vs 3 (10%)], delayed discharge of more than belief that a double application of the harmonic shears to the
2 days was only for one patient in group I [1 (3.3%) cystic duct is unnecessary and may be an unsafe practice.
(p-value = 0.13)]. The mean hospital stay in group II The greater cost of the harmonic scalpel, when com-
(1.1 ± 0.30) is less than that in group I (1.33 ± 0.54) with pared with the cost of an electrocautery probe, has been
statistical significance (p-value = 0.046) (Table 4). regarded as a potential disadvantage. Although this
Three months after the procedure, all patients were difference is significant at the present time, however, we
doing well with uneventful follow-up. feel that LC, using the harmonic scalpel, is cost-effective
when considering that we use fewer overall instruments
and are able to carry out more procedures on an average
DISCUSSION
list as a result of the shorter operative time.
Several studies have confirmed the effectiveness and The overall hospital stay in group II is less than
11
safety of the use of the ultrasonically activated scalpel for group I, similar to the Janssen et al study which reported
20