Page 63 - World Journal of Laparoscopic Surgery
P. 63
Laparoscopic Cholecystectomy: How We Do It
Figs 1A and B: (A) Enlarged left liver lobe; (B) Shuttering Calot’s triangle and post-dissection view
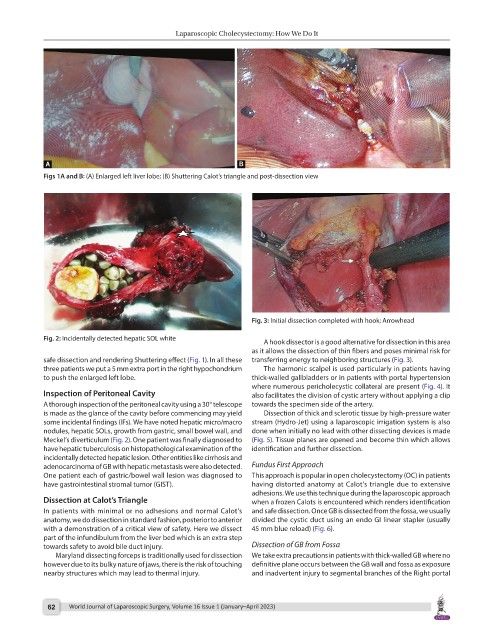
Fig. 3: Initial dissection completed with hook; Arrowhead
Fig. 2: Incidentally detected hepatic SOL white
A hook dissector is a good alternative for dissection in this area
as it allows the dissection of thin fibers and poses minimal risk for
safe dissection and rendering Shuttering effect (Fig. 1). In all these transferring energy to neighboring structures (Fig. 3).
three patients we put a 5 mm extra port in the right hypochondrium The harmonic scalpel is used particularly in patients having
to push the enlarged left lobe. thick-walled gallbladders or in patients with portal hypertension
where numerous pericholecystic collateral are present (Fig. 4). It
Inspection of Peritoneal Cavity also facilitates the division of cystic artery without applying a clip
A thorough inspection of the peritoneal cavity using a 30°telescope towards the specimen side of the artery.
is made as the glance of the cavity before commencing may yield Dissection of thick and sclerotic tissue by high-pressure water
some incidental findings (IFs). We have noted hepatic micro/macro stream (Hydro-Jet) using a laparoscopic irrigation system is also
nodules, hepatic SOLs, growth from gastric, small bowel wall, and done when initially no lead with other dissecting devices is made
Meckel’s diverticulum (Fig. 2). One patient was finally diagnosed to (Fig. 5). Tissue planes are opened and become thin which allows
have hepatic tuberculosis on histopathological examination of the identification and further dissection.
incidentally detected hepatic lesion. Other entities like cirrhosis and
adenocarcinoma of GB with hepatic metastasis were also detected. Fundus First Approach
One patient each of gastric/bowel wall lesion was diagnosed to This approach is popular in open cholecystectomy (OC) in patients
have gastrointestinal stromal tumor (GIST). having distorted anatomy at Calot’s triangle due to extensive
adhesions. We use this technique during the laparoscopic approach
Dissection at Calot’s Triangle when a frozen Calots is encountered which renders identification
In patients with minimal or no adhesions and normal Calot’s and safe dissection. Once GB is dissected from the fossa, we usually
anatomy, we do dissection in standard fashion, posterior to anterior divided the cystic duct using an endo GI linear stapler (usually
with a demonstration of a critical view of safety. Here we dissect 45 mm blue reload) (Fig. 6).
part of the infundibulum from the liver bed which is an extra step
towards safety to avoid bile duct injury. Dissection of GB from Fossa
Maryland dissecting forceps is traditionally used for dissection We take extra precautions in patients with thick-walled GB where no
however due to its bulky nature of jaws, there is the risk of touching definitive plane occurs between the GB wall and fossa as exposure
nearby structures which may lead to thermal injury. and inadvertent injury to segmental branches of the Right portal
62 World Journal of Laparoscopic Surgery, Volume 16 Issue 1 (January–April 2023)