Page 78 - World Journal of Laparoscopic Surgery
P. 78
Laparoscopic Spleen-preserving Distal Pancreatectomy for Trauma
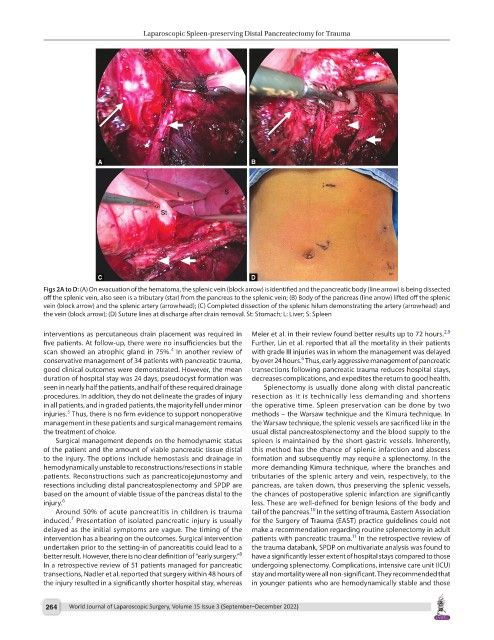
Figs 2A to D: (A) On evacuation of the hematoma, the splenic vein (block arrow) is identified and the pancreatic body (line arrow) is being dissected
off the splenic vein, also seen is a tributary (star) from the pancreas to the splenic vein; (B) Body of the pancreas (line arrow) lifted off the splenic
vein (block arrow) and the splenic artery (arrowhead); (C) Completed dissection of the splenic hilum demonstrating the artery (arrowhead) and
the vein (block arrow); (D) Suture lines at discharge after drain removal. St: Stomach; L: Liver; S: Spleen
2,9
interventions as percutaneous drain placement was required in Meier et al. in their review found better results up to 72 hours.
five patients. At follow-up, there were no insufficiencies but the Further, Lin et al. reported that all the mortality in their patients
4
scan showed an atrophic gland in 75%. In another review of with grade III injuries was in whom the management was delayed
6
conservative management of 34 patients with pancreatic trauma, by over 24 hours. Thus, early aggressive management of pancreatic
good clinical outcomes were demonstrated. However, the mean transections following pancreatic trauma reduces hospital stays,
duration of hospital stay was 24 days, pseudocyst formation was decreases complications, and expedites the return to good health.
seen in nearly half the patients, and half of these required drainage Splenectomy is usually done along with distal pancreatic
procedures. In addition, they do not delineate the grades of injury resection as it is technically less demanding and shortens
in all patients, and in graded patients, the majority fell under minor the operative time. Spleen preservation can be done by two
5
injuries. Thus, there is no firm evidence to support nonoperative methods – the Warsaw technique and the Kimura technique. In
management in these patients and surgical management remains the Warsaw technique, the splenic vessels are sacrificed like in the
the treatment of choice. usual distal pancreatosplenectomy and the blood supply to the
Surgical management depends on the hemodynamic status spleen is maintained by the short gastric vessels. Inherently,
of the patient and the amount of viable pancreatic tissue distal this method has the chance of splenic infarction and abscess
to the injury. The options include hemostasis and drainage in formation and subsequently may require a splenectomy. In the
hemodynamically unstable to reconstructions/resections in stable more demanding Kimura technique, where the branches and
patients. Reconstructions such as pancreaticojejunostomy and tributaries of the splenic artery and vein, respectively, to the
resections including distal pancreatosplenectomy and SPDP are pancreas, are taken down, thus preserving the splenic vessels,
based on the amount of viable tissue of the pancreas distal to the the chances of postoperative splenic infarction are significantly
injury. 6 less. These are well-defined for benign lesions of the body and
10
Around 50% of acute pancreatitis in children is trauma tail of the pancreas. In the setting of trauma, Eastern Association
7
induced. Presentation of isolated pancreatic injury is usually for the Surgery of Trauma (EAST) practice guidelines could not
delayed as the initial symptoms are vague. The timing of the make a recommendation regarding routine splenectomy in adult
11
intervention has a bearing on the outcomes. Surgical intervention patients with pancreatic trauma. In the retrospective review of
undertaken prior to the setting-in of pancreatitis could lead to a the trauma databank, SPDP on multivariate analysis was found to
8
better result. However, there is no clear definition of “early surgery.” have a significantly lesser extent of hospital stays compared to those
In a retrospective review of 51 patients managed for pancreatic undergoing splenectomy. Complications, intensive care unit (ICU)
transections, Nadler et al. reported that surgery within 48 hours of stay and mortality were all non-significant. They recommended that
the injury resulted in a significantly shorter hospital stay, whereas in younger patients who are hemodynamically stable and those
264 World Journal of Laparoscopic Surgery, Volume 15 Issue 3 (September–December 2022)