Page 77 - World Journal of Laparoscopic Surgery
P. 77
Laparoscopic Spleen-preserving Distal Pancreatectomy for Trauma
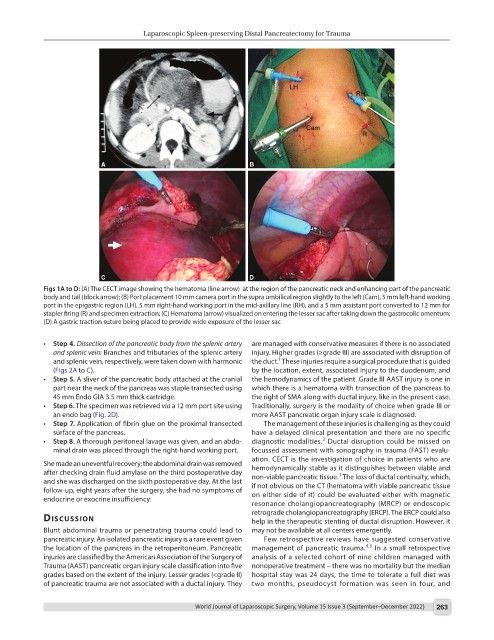
Figs 1A to D: (A) The CECT image showing the hematoma (line arrow) at the region of the pancreatic neck and enhancing part of the pancreatic
body and tail (block arrow); (B) Port placement 10 mm camera port in the supra umbilical region slightly to the left (Cam), 5 mm left-hand working
port in the epigastric region (LH), 5 mm right-hand working port in the mid-axillary line (RH), and a 5 mm assistant port converted to 12 mm for
stapler firing (R) and specimen extraction; (C) Hematoma (arrow) visualized on entering the lesser sac after taking down the gastrocolic omentum;
(D) A gastric traction suture being placed to provide wide exposure of the lesser sac
• Step 4. Dissection of the pancreatic body from the splenic artery are managed with conservative measures if there is no associated
and splenic vein: Branches and tributaries of the splenic artery injury. Higher grades (≥grade III) are associated with disruption of
1
and splenic vein, respectively, were taken down with harmonic the duct. These injuries require a surgical procedure that is guided
(Figs 2A to C). by the location, extent, associated injury to the duodenum, and
• Step 5. A sliver of the pancreatic body attached at the cranial the hemodynamics of the patient. Grade III AAST injury is one in
part near the neck of the pancreas was staple transected using which there is a hematoma with transection of the pancreas to
45 mm Endo GIA 3.5 mm thick cartridge. the right of SMA along with ductal injury, like in the present case.
• Step 6. The specimen was retrieved via a 12 mm port site using Traditionally, surgery is the modality of choice when grade III or
an endo bag (Fig. 2D). more AAST pancreatic organ injury scale is diagnosed.
• Step 7. Application of fibrin glue on the proximal transected The management of these injuries is challenging as they could
surface of the pancreas. have a delayed clinical presentation and there are no specific
2
• Step 8. A thorough peritoneal lavage was given, and an abdo- diagnostic modalities. Ductal disruption could be missed on
minal drain was placed through the right-hand working port. focussed assessment with sonography in trauma (FAST) evalu-
ation. CECT is the investigation of choice in patients who are
She made an uneventful recovery; the abdominal drain was removed
after checking drain fluid amylase on the third postoperative day hemodynamically stable as it distinguishes between viable and
3
and she was discharged on the sixth postoperative day. At the last non-viable pancreatic tissue. The loss of ductal continuity, which,
follow-up, eight years after the surgery, she had no symptoms of if not obvious on the CT (hematoma with viable pancreatic tissue
endocrine or exocrine insufficiency. on either side of it) could be evaluated either with magnetic
resonance cholangiopancreatography (MRCP) or endoscopic
retrograde cholangiopancreatography (ERCP). The ERCP could also
discussion help in the therapeutic stenting of ductal disruption. However, it
Blunt abdominal trauma or penetrating trauma could lead to may not be available at all centers emergently.
pancreatic injury. An isolated pancreatic injury is a rare event given Few retrospective reviews have suggested conservative
4,5
the location of the pancreas in the retroperitoneum. Pancreatic management of pancreatic trauma. In a small retrospective
injuries are classified by the American Association of the Surgery of analysis of a selected cohort of nine children managed with
Trauma (AAST) pancreatic organ injury scale classification into five nonoperative treatment – there was no mortality but the median
grades based on the extent of the injury. Lesser grades (<grade II) hospital stay was 24 days, the time to tolerate a full diet was
of pancreatic trauma are not associated with a ductal injury. They two months, pseudocyst formation was seen in four, and
World Journal of Laparoscopic Surgery, Volume 15 Issue 3 (September–December 2022) 263