Page 22 - World Journal of Laparoscopic Surgery
P. 22
Role of Hysterolaparoscopy in Evaluation of Subfertility
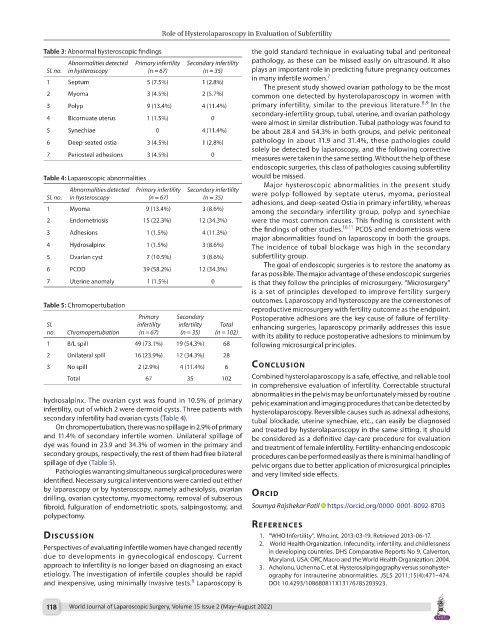
Table 3: Abnormal hysteroscopic findings the gold standard technique in evaluating tubal and peritoneal
Abnormalities detected Primary infertility Secondary infertility pathology, as these can be missed easily on ultrasound. It also
Sl. no. in hysteroscopy (n = 67) (n = 35) plays an important role in predicting future pregnancy outcomes
in many infertile women. 7
1 Septum 5 (7.5%) 1 (2.8%)
The present study showed ovarian pathology to be the most
2 Myoma 3 (4.5%) 2 (5.7%) common one detected by hysterolaparoscopy in women with
8,9
3 Polyp 9 (13.4%) 4 (11.4%) primary infertility, similar to the previous literature. In the
secondary-infertility group, tubal, uterine, and ovarian pathology
4 Bicornuate uterus 1 (1.5%) 0
were almost in similar distribution. Tubal pathology was found to
5 Synechiae 0 4 (11.4%) be about 28.4 and 54.3% in both groups, and pelvic peritoneal
6 Deep-seated ostia 3 (4.5%) 1 (2.8%) pathology in about 11.9 and 31.4%, these pathologies could
solely be detected by laparoscopy, and the following corrective
7 Periosteal adhesions 3 (4.5%) 0
measures were taken in the same setting. Without the help of these
endoscopic surgeries, this class of pathologies causing subfertility
Table 4: Laparoscopic abnormalities would be missed.
Major hysteroscopic abnormalities in the present study
Abnormalities detected Primary infertility Secondary infertility were polyp followed by septate uterus, myoma, periosteal
Sl. no. in hysteroscopy (n = 67) (n = 35)
adhesions, and deep-seated Ostia in primary infertility, whereas
1 Myoma 9 (13.4%) 3 (8.6%) among the secondary infertility group, polyp and synechiae
2 Endometriosis 15 (22.3%) 12 (34.3%) were the most common causes. This finding is consistent with
the findings of other studies. 10,11 PCOS and endometriosis were
3 Adhesions 1 (1.5%) 4 (11.3%)
major abnormalities found on laparoscopy in both the groups.
4 Hydrosalpinx 1 (1.5%) 3 (8.6%) The incidence of tubal blockage was high in the secondary
5 Ovarian cyst 7 (10.5%) 3 (8.6%) subfertility group.
The goal of endoscopic surgeries is to restore the anatomy as
6 PCOD 39 (58.2%) 12 (34.3%)
far as possible. The major advantage of these endoscopic surgeries
7 Uterine anomaly 1 (1.5%) 0 is that they follow the principles of microsurgery. “Microsurgery”
is a set of principles developed to improve fertility surgery
outcomes. Laparoscopy and hysteroscopy are the cornerstones of
Table 5: Chromopertubation
reproductive microsurgery with fertility outcome as the endpoint.
Primary Secondary Postoperative adhesions are the key cause of failure of fertility-
Sl. infertility infertility Total enhancing surgeries, laparoscopy primarily addresses this issue
no. Chromopertubation (n = 67) (n = 35) (n = 102)
with its ability to reduce postoperative adhesions to minimum by
1 B/L spill 49 (73.1%) 19 (54.3%) 68 following microsurgical principles.
2 Unilateral spill 16 (23.9%) 12 (34.3%) 28
3 No spill 2 (2.9%) 4 (11.4%) 6 conclusIon
Total 67 35 102 Combined hysterolaparoscopy is a safe, effective, and reliable tool
in comprehensive evaluation of infertility. Correctable structural
abnormalities in the pelvis may be unfortunately missed by routine
hydrosalpinx. The ovarian cyst was found in 10.5% of primary pelvic examination and imaging procedures that can be detected by
infertility, out of which 2 were dermoid cysts. Three patients with hysterolaparoscopy. Reversible causes such as adnexal adhesions,
secondary infertility had ovarian cysts (Table 4). tubal blockade, uterine synechiae, etc., can easily be diagnosed
On chromopertubation, there was no spillage in 2.9% of primary and treated by hysterolaparoscopy in the same sitting. It should
and 11.4% of secondary infertile women. Unilateral spillage of be considered as a definitive day-care procedure for evaluation
dye was found in 23.9 and 34.3% of women in the primary and and treatment of female infertility. Fertility-enhancing endoscopic
secondary groups, respectively, the rest of them had free bilateral procedures can be performed easily as there is minimal handling of
spillage of dye (Table 5). pelvic organs due to better application of microsurgical principles
Pathologies warranting simultaneous surgical procedures were and very limited side effects.
identified. Necessary surgical interventions were carried out either
by laparoscopy or by hysteroscopy, namely adhesiolysis, ovarian orcId
drilling, ovarian cystectomy, myomectomy, removal of subserous
fibroid, fulguration of endometriotic spots, salpingostomy, and Soumya Rajshekar Patil https://orcid.org/0000-0001-8092-8703
polypectomy.
references
dIscussIon 1. “WHO Infertility”. Who.int. 2013-03-19. Retrieved 2013-06-17.
2. World Health Organization. Infecundity, infertility, and childlessness
Perspectives of evaluating infertile women have changed recently
due to developments in gynecological endoscopy. Current in developing countries. DHS Comparative Reports No 9. Calverton,
Maryland, USA: ORC Macro and the World Health Organization; 2004.
approach to infertility is no longer based on diagnosing an exact 3. Acholonu, Uchenna C, et al. Hysterosalpingography versus sonohyster-
etiology. The investigation of infertile couples should be rapid ography for intrauterine abnormalities. JSLS 2011;15(4):471–474.
6
and inexpensive, using minimally invasive tests. Laparoscopy is DOI: 10.4293/108680811X13176785203923.
118 World Journal of Laparoscopic Surgery, Volume 15 Issue 2 (May–August 2022)