Page 25 - World Journal of Laparoscopic Surgery
P. 25
Is Previous Abdominal or Pelvic Surgery a Risk Factor?
of grasping prongs at the distal end. Preloaded silastic-ring
applicator was introduced through the lateral port and fallopian
tube grasped approximately 3 cm distal to cornual end. Adequate
knuckle of the tube was approximately 1 cm long with an obvious
inner loop. Applicators are available that can accommodate one
or two rings at a later time, one could be beneficial as reloading
between the banding can be prevented. Difficulty with silastic-ring
placement was observed with adherent or edematous tubes, where
the “Yoon three grasp technique” was used for ring placement.
Postoperatively, knuckle of the tube undergoes necrosis from blood
supply interruption, and within a span of 3–6 months, complete
absorption of knuckle occurs and proximal and distal stumps
separate completely.
Statistical Analysis
The data on categorical variables are shown as n (% of cases). All
results are shown in graphical format.
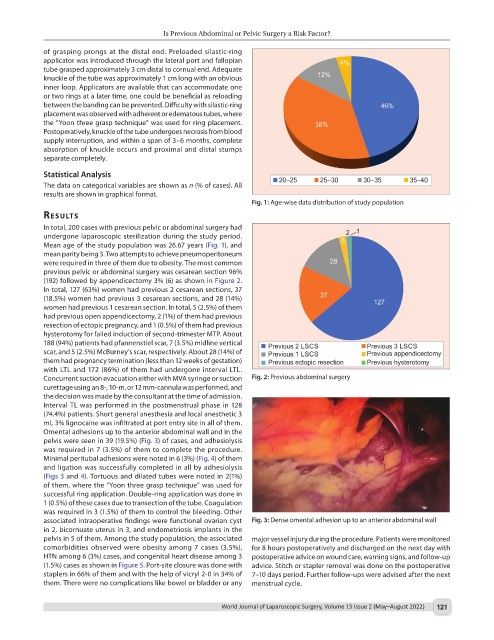
Fig. 1: Age-wise data distribution of study population
results
In total, 200 cases with previous pelvic or abdominal surgery had
undergone laparoscopic sterilization during the study period.
Mean age of the study population was 26.67 years (Fig. 1), and
mean parity being 3. Two attempts to achieve pneumoperitoneum
were required in three of them due to obesity. The most common
previous pelvic or abdominal surgery was cesarean section 96%
(192) followed by appendicectomy 3% (6) as shown in Figure 2.
In total, 127 (63%) women had previous 2 cesarean sections, 37
(18.5%) women had previous 3 cesarean sections, and 28 (14%)
women had previous 1 cesarean section. In total, 5 (2.5%) of them
had previous open appendicectomy, 2 (1%) of them had previous
resection of ectopic pregnancy, and 1 (0.5%) of them had previous
hysterotomy for failed induction of second-trimester MTP. About
188 (94%) patients had pfannenstiel scar, 7 (3.5%) midline vertical
scar, and 5 (2.5%) McBurney’s scar, respectively. About 28 (14%) of
them had pregnancy termination (less than 12 weeks of gestation)
with LTL and 172 (86%) of them had undergone interval LTL.
Concurrent suction evacuation either with MVA syringe or suction Fig. 2: Previous abdominal surgery
curettage using an 8-, 10-m, or 12 mm-cannula was performed, and
the decision was made by the consultant at the time of admission.
Interval TL was performed in the postmenstrual phase in 128
(74.4%) patients. Short general anesthesia and local anesthetic 3
mL 3% lignocaine was infiltrated at port entry site in all of them.
Omental adhesions up to the anterior abdominal wall and in the
pelvis were seen in 39 (19.5%) (Fig. 3) of cases, and adhesiolysis
was required in 7 (3.5%) of them to complete the procedure.
Minimal peritubal adhesions were noted in 6 (3%) (Fig. 4) of them
and ligation was successfully completed in all by adhesiolysis
(Figs 3 and 4). Tortuous and dilated tubes were noted in 2(1%)
of them, where the “Yoon three grasp technique” was used for
successful ring application. Double-ring application was done in
1 (0.5%) of these cases due to transection of the tube. Coagulation
was required in 3 (1.5%) of them to control the bleeding. Other
associated intraoperative findings were functional ovarian cyst Fig. 3: Dense omental adhesion up to an anterior abdominal wall
in 2, bicornuate uterus in 3, and endometriosis implants in the
pelvis in 5 of them. Among the study population, the associated major vessel injury during the procedure. Patients were monitored
comorbidities observed were obesity among 7 cases (3.5%), for 8 hours postoperatively and discharged on the next day with
HTN among 6 (3%) cases, and congenital heart disease among 3 postoperative advice on wound care, warning signs, and follow-up
(1.5%) cases as shown in Figure 5. Port-site closure was done with advice. Stitch or stapler removal was done on the postoperative
staplers in 66% of them and with the help of vicryl 2-0 in 34% of 7–10 days period. Further follow-ups were advised after the next
them. There were no complications like bowel or bladder or any menstrual cycle.
World Journal of Laparoscopic Surgery, Volume 15 Issue 2 (May–August 2022) 121