Page 6 - World Journal of Laparoscopic Surgery
P. 6
Conversion of LC to Open Surgery
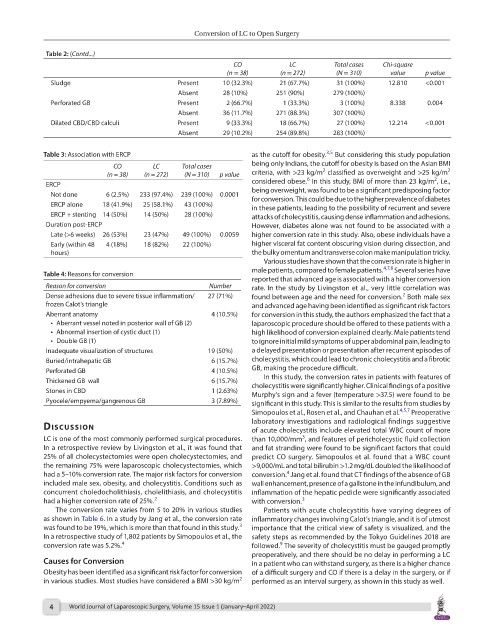
Table 2: (Contd...)
CO LC Total cases Chi-square
(n = 38) (n = 272) (N = 310) value p value
Sludge Present 10 (32.3%) 21 (67.7%) 31 (100%) 12.810 <0.001
Absent 28 (10%) 251 (90%) 279 (100%)
Perforated GB Present 2 (66.7%) 1 (33.3%) 3 (100%) 8.338 0.004
Absent 36 (11.7%) 271 (88.3%) 307 (100%)
Dilated CBD/CBD calculi Present 9 (33.3%) 18 (66.7%) 27 (100%) 12.214 <0.001
Absent 29 (10.2%) 254 (89.8%) 283 (100%)
3,5
Table 3: Association with ERCP as the cutoff for obesity. But considering this study population
CO LC Total cases being only Indians, the cutoff for obesity is based on the Asian BMI
2
2
(n = 38) (n = 272) (N = 310) p value criteria, with >23 kg/m classified as overweight and >25 kg/m
6
2
ERCP considered obese. In this study, BMI of more than 23 kg/m , i.e.,
Not done 6 (2.5%) 233 (97.4%) 239 (100%) 0.0001 being overweight, was found to be a significant predisposing factor
for conversion. This could be due to the higher prevalence of diabetes
ERCP alone 18 (41.9%) 25 (58.1%) 43 (100%) in these patients, leading to the possibility of recurrent and severe
ERCP + stenting 14 (50%) 14 (50%) 28 (100%) attacks of cholecystitis, causing dense inflammation and adhesions.
Duration post-ERCP However, diabetes alone was not found to be associated with a
Late (>6 weeks) 26 (53%) 23 (47%) 49 (100%) 0.0059 higher conversion rate in this study. Also, obese individuals have a
Early (within 48 4 (18%) 18 (82%) 22 (100%) higher visceral fat content obscuring vision during dissection, and
hours) the bulky omentum and transverse colon make manipulation tricky.
Various studies have shown that the conversion rate is higher in
male patients, compared to female patients. 4,7,8 Several series have
Table 4: Reasons for conversion
reported that advanced age is associated with a higher conversion
Reason for conversion Number rate. In the study by Livingston et al., very little correlation was
Dense adhesions due to severe tissue inflammation/ 27 (71%) found between age and the need for conversion. Both male sex
2
frozen Calot’s triangle and advanced age having been identified as significant risk factors
Aberrant anatomy 4 (10.5%) for conversion in this study, the authors emphasized the fact that a
• Aberrant vessel noted in posterior wall of GB (2) laparoscopic procedure should be offered to these patients with a
• Abnormal insertion of cystic duct (1) high likelihood of conversion explained clearly. Male patients tend
• Double GB (1) to ignore initial mild symptoms of upper abdominal pain, leading to
Inadequate visualization of structures 19 (50%) a delayed presentation or presentation after recurrent episodes of
Buried/intrahepatic GB 6 (15.7%) cholecystitis, which could lead to chronic cholecystitis and a fibrotic
Perforated GB 4 (10.5%) GB, making the procedure difficult.
In this study, the conversion rates in patients with features of
Thickened GB wall 6 (15.7%) cholecystitis were significantly higher. Clinical findings of a positive
Stones in CBD 1 (2.63%) Murphy’s sign and a fever (temperature >37.5) were found to be
Pyocele/empyema/gangrenous GB 3 (7.89%) significant in this study. This is similar to the results from studies by
Simopoulos et al., Rosen et al., and Chauhan et al. 4,5,7 Preoperative
laboratory investigations and radiological findings suggestive
dIscussIon of acute cholecystitis include elevated total WBC count of more
3
LC is one of the most commonly performed surgical procedures. than 10,000/mm , and features of pericholecystic fluid collection
In a retrospective review by Livingston et al., it was found that and fat stranding were found to be significant factors that could
25% of all cholecystectomies were open cholecystectomies, and predict CO surgery. Simopoulos et al. found that a WBC count
the remaining 75% were laparoscopic cholecystectomies, which >9,000/mL and total bilirubin >1.2 mg/dL doubled the likelihood of
4
had a 5–10% conversion rate. The major risk factors for conversion conversion. Jang et al. found that CT findings of the absence of GB
included male sex, obesity, and cholecystitis. Conditions such as wall enhancement, presence of a gallstone in the infundibulum, and
concurrent choledocholithiasis, cholelithiasis, and cholecystitis inflammation of the hepatic pedicle were significantly associated
had a higher conversion rate of 25%. 2 with conversion. 3
The conversion rate varies from 5 to 20% in various studies Patients with acute cholecystitis have varying degrees of
as shown in Table 6. In a study by Jang et al., the conversion rate inflammatory changes involving Calot’s triangle, and it is of utmost
3
was found to be 19%, which is more than that found in this study. importance that the critical view of safety is visualized, and the
In a retrospective study of 1,802 patients by Simopoulos et al., the safety steps as recommended by the Tokyo Guidelines 2018 are
conversion rate was 5.2%. 4 followed. The severity of cholecystitis must be gauged promptly
9
preoperatively, and there should be no delay in performing a LC
Causes for Conversion in a patient who can withstand surgery, as there is a higher chance
Obesity has been identified as a significant risk factor for conversion of a difficult surgery and CO if there is a delay in the surgery, or if
2
in various studies. Most studies have considered a BMI >30 kg/m performed as an interval surgery, as shown in this study as well.
4 World Journal of Laparoscopic Surgery, Volume 15 Issue 1 (January–April 2022)