Page 32 - tmp
P. 32
Evaluation of Open vs Laparoscopic Pyeloplasty in Children
thorough history is collected, including age, gender, stomach
discomfort, fever, and urinary tract infections. It was also necessary
to gather information about one’s past and family history.
Procedure
Open Pyeloplasty
It is feasible to perform this procedure through a variety of
incisions, but we went with an extraperitoneal flank incision. The
restricted UPJ segment is surgically removed, and the renal pelvis
is anastomosed to the spatulated upper ureter. Assuming the renal
pelvis is extensively dilated; in this case, it was regularly reduced in
size by chopping off unneeded tissue. It is then sutured such that
it streamlines down toward the anastomosis, and a double J stent
and a flank drain are placed across the anastomosis. They were
removed 48–72 hours following surgery. If a vascular abnormality
is discovered near the UPJ, the anastomosis is done anterior to the
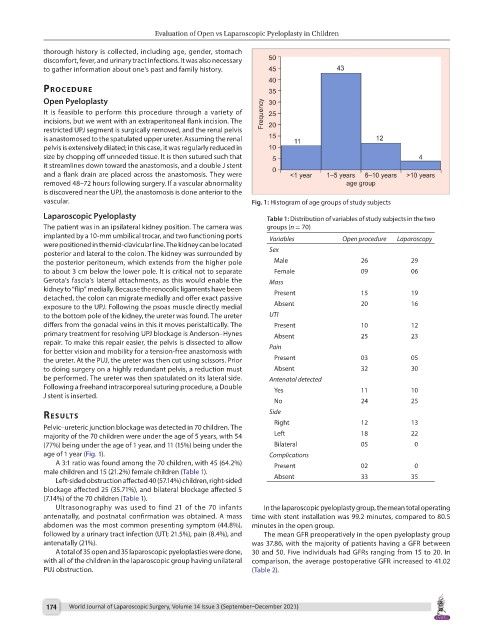
vascular. Fig. 1: Histogram of age groups of study subjects
Laparoscopic Pyeloplasty Table 1: Distribution of variables of study subjects in the two
The patient was in an ipsilateral kidney position. The camera was groups (n = 70)
implanted by a 10-mm umbilical trocar, and two functioning ports Variables Open procedure Laparoscopy
were positioned in the mid-clavicular line. The kidney can be located
posterior and lateral to the colon. The kidney was surrounded by Sex
the posterior peritoneum, which extends from the higher pole Male 26 29
to about 3 cm below the lower pole. It is critical not to separate Female 09 06
Gerota’s fascia’s lateral attachments, as this would enable the Mass
kidney to “flip” medially. Because the renocolic ligaments have been Present 15 19
detached, the colon can migrate medially and offer exact passive
exposure to the UPJ. Following the psoas muscle directly medial Absent 20 16
to the bottom pole of the kidney, the ureter was found. The ureter UTI
differs from the gonadal veins in this it moves peristaltically. The Present 10 12
primary treatment for resolving UPJ blockage is Anderson–Hynes Absent 25 23
repair. To make this repair easier, the pelvis is dissected to allow
for better vision and mobility for a tension-free anastomosis with Pain
the ureter. At the PUJ, the ureter was then cut using scissors. Prior Present 03 05
to doing surgery on a highly redundant pelvis, a reduction must Absent 32 30
be performed. The ureter was then spatulated on its lateral side. Antenatal detected
Following a freehand intracorporeal suturing procedure, a Double Yes 11 10
J stent is inserted.
No 24 25
Side
results
Pelvic–ureteric junction blockage was detected in 70 children. The Right 12 13
majority of the 70 children were under the age of 5 years, with 54 Left 18 22
(77%) being under the age of 1 year, and 11 (15%) being under the Bilateral 05 0
age of 1 year (Fig. 1). Complications
A 3:1 ratio was found among the 70 children, with 45 (64.2%) Present 02 0
male children and 15 (21.2%) female children (Table 1).
Left-sided obstruction affected 40 (57.14%) children, right-sided Absent 33 35
blockage affected 25 (35.71%), and bilateral blockage affected 5
(7.14%) of the 70 children (Table 1).
Ultrasonography was used to find 21 of the 70 infants In the laparoscopic pyeloplasty group, the mean total operating
antenatally, and postnatal confirmation was obtained. A mass time with stent installation was 99.2 minutes, compared to 80.5
abdomen was the most common presenting symptom (44.8%), minutes in the open group.
followed by a urinary tract infection (UTI; 21.5%), pain (8.4%), and The mean GFR preoperatively in the open pyeloplasty group
antenatally (21%). was 37.86, with the majority of patients having a GFR between
A total of 35 open and 35 laparoscopic pyeloplasties were done, 30 and 50. Five individuals had GFRs ranging from 15 to 20. In
with all of the children in the laparoscopic group having unilateral comparison, the average postoperative GFR increased to 41.02
PUJ obstruction. (Table 2).
174 World Journal of Laparoscopic Surgery, Volume 14 Issue 3 (September–December 2021)