Page 34 - World Journal of Laparoscopic Surgery
P. 34
A Comparative Evaluation of Total Laparoscopic Hysterectomy and Laparoscopic Supracervical Hysterectomy
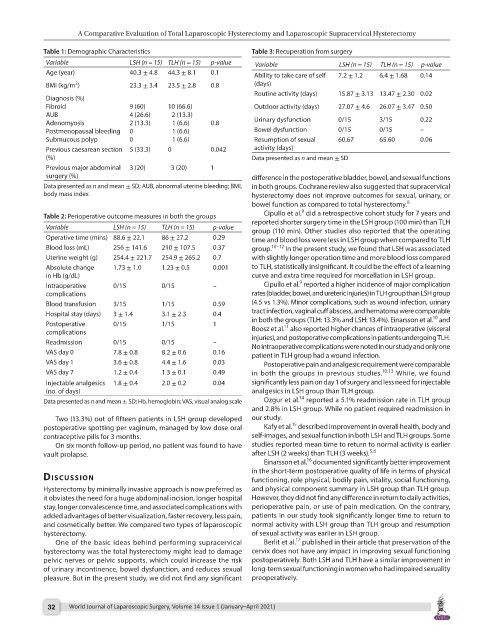
Table 1: Demographic Characteristics Table 3: Recuperation from surgery
Variable LSH (n = 15) TLH (n = 15) p-value Variable LSH (n = 15) TLH (n = 15) p-value
Age (year) 40.3 ± 4.8 44.3 ± 8.1 0.1 Ability to take care of self 7.2 ± 1.2 6.4 ± 1.68 0.14
2
BMI (kg/m ) 23.3 ± 3.4 23.5 ± 2.8 0.8 (days)
Routine activity (days) 15.87 ± 3.13 13.47 ± 2.30 0.02
Diagnosis (%)
Fibroid 9 (60) 10 (66.6) Outdoor activity (days) 27.07 ± 4.6 26.07 ± 3.47 0.50
AUB 4 (26.6) 2 (13.3)
Adenomyosis 2 (13.3) 1 (6.6) 0.8 Urinary dysfunction 0/15 3/15 0.22
Postmenopausal bleeding 0 1 (6.6) Bowel dysfunction 0/15 0/15 –
Submucous polyp 0 1 (6.6) Resumption of sexual 60.67 65.60 0.06
Previous caesarean section 5 (33.3) 0 0.042 activity (days)
(%) Data presented as n and mean ± SD
Previous major abdominal 3 (20) 3 (20) 1
surgery (%) difference in the postoperative bladder, bowel, and sexual functions
Data presented as n and mean ± SD; AUB, abnormal uterine bleeding; BMI, in both groups. Cochrane review also suggested that supracervical
body mass index hysterectomy does not improve outcomes for sexual, urinary, or
bowel function as compared to total hysterectomy. 8
9
Table 2: Perioperative outcome measures in both the groups Cipullo et al. did a retrospective cohort study for 7 years and
reported shorter surgery time in the LSH group (100 min) than TLH
Variable LSH (n = 15) TLH (n = 15) p-value group (110 min). Other studies also reported that the operating
Operative time (mins) 88.6 ± 22.1 86 ± 27.2 0.29 time and blood loss were less in LSH group when compared to TLH
Blood loss (mL) 256 ± 141.6 210 ± 107.5 0.37 group. 10–12 In the present study, we found that LSH was associated
Uterine weight (g) 254.4 ± 221.7 254.9 ± 265.2 0.7 with slightly longer operation time and more blood loss compared
Absolute change 1.73 ± 1.0 1.23 ± 0.5 0.001 to TLH, statistically insignificant. It could be the effect of a learning
in Hb (g/dL) curve and extra time required for morcellation in LSH group.
9
Intraoperative 0/15 0/15 – Cipullo et al. reported a higher incidence of major complication
complications rates (bladder, bowel, and ureteric injuries) in TLH group than LSH group
Blood transfusion 3/15 1/15 0.59 (4.5 vs 1.3%). Minor complications, such as wound infection, urinary
Hospital stay (days) 3 ± 1.4 3.1 ± 2.3 0.4 tract infection, vaginal cuff abscess, and hematoma were comparable
10
Postoperative 0/15 1/15 1 in both the groups (TLH: 13.3% and LSH: 13.4%). Einarsson et al. and
11
Boosz et al. also reported higher chances of intraoperative (visceral
complications injuries), and postoperative complications in patients undergoing TLH.
Readmission 0/15 0/15 – No intraoperative complications were noted in our study and only one
VAS day 0 7.8 ± 0.8 8.2 ± 0.6 0.16 patient in TLH group had a wound infection.
VAS day 1 3.6 ± 0.8 4.4 ± 1.6 0.03 Postoperative pain and analgesic requirement were comparable
VAS day 7 1.2 ± 0.4 1.3 ± 0.1 0.49 in both the groups in previous studies. 10,13 While, we found
Injectable analgesics 1.8 ± 0.4 2.0 ± 0.2 0.04 significantly less pain on day 1 of surgery and less need for injectable
(no. of days) analgesics in LSH group than TLH group.
14
Data presented as n and mean ± SD; Hb, hemoglobin; VAS, visual analog scale Ozgur et al. reported a 5.1% readmission rate in TLH group
and 2.8% in LSH group. While no patient required readmission in
Two (13.3%) out of fifteen patients in LSH group developed our study.
15
postoperative spotting per vaginum, managed by low dose oral Kafy et al. described improvement in overall health, body and
contraceptive pills for 3 months. self-images, and sexual function in both LSH and TLH groups. Some
On six month follow-up period, no patient was found to have studies reported mean time to return to normal activity is earlier
5,6
vault prolapse. after LSH (2 weeks) than TLH (3 weeks).
16
Einarsson et al. documented significantly better improvement
in the short-term postoperative quality of life in terms of physical
discussion functioning, role physical, bodily pain, vitality, social functioning,
Hysterectomy by minimally invasive approach is now preferred as and physical component summary in LSH group than TLH group.
it obviates the need for a huge abdominal incision, longer hospital However, they did not find any difference in return to daily activities,
stay, longer convalescence time, and associated complications with perioperative pain, or use of pain medication. On the contrary,
added advantages of better visualization, faster recovery, less pain, patients in our study took significantly longer time to return to
and cosmetically better. We compared two types of laparoscopic normal activity with LSH group than TLH group and resumption
hysterectomy. of sexual activity was earlier in LSH group.
17
One of the basic ideas behind performing supracervical Berlit et al. published in their article that preservation of the
hysterectomy was the total hysterectomy might lead to damage cervix does not have any impact in improving sexual functioning
pelvic nerves or pelvic supports, which could increase the risk postoperatively. Both LSH and TLH have a similar improvement in
of urinary incontinence, bowel dysfunction, and reduces sexual long-term sexual functioning in women who had impaired sexuality
pleasure. But in the present study, we did not find any significant preoperatively.
32 World Journal of Laparoscopic Surgery, Volume 14 Issue 1 (January–April 2021)