Page 29 - World Journal of Laparoscopic Surgery
P. 29
Comparative Outcome of LGI, LSG and LRYGB for Weight Loss and BMI Reduction
2
2
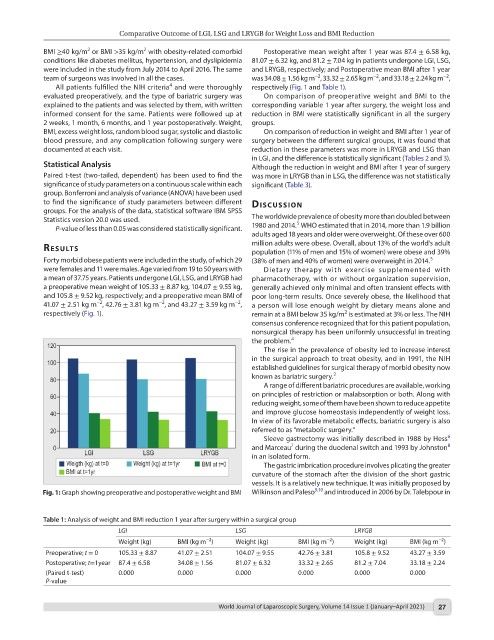
BMI ≥40 kg/m or BMI >35 kg/m with obesity-related comorbid Postoperative mean weight after 1 year was 87.4 ± 6.58 kg,
conditions like diabetes mellitus, hypertension, and dyslipidemia 81.07 ± 6.32 kg, and 81.2 ± 7.04 kg in patients undergone LGI, LSG,
were included in the study from July 2014 to April 2016. The same and LRYGB, respectively; and Postoperative mean BMI after 1 year
−2
−2
−2
team of surgeons was involved in all the cases. was 34.08 ± 1.56 kg m , 33.32 ± 2.65 kg m , and 33.18 ± 2.24 kg m ,
4
All patients fulfilled the NIH criteria and were thoroughly respectively (Fig. 1 and Table 1).
evaluated preoperatively, and the type of bariatric surgery was On comparison of preoperative weight and BMI to the
explained to the patients and was selected by them, with written corresponding variable 1 year after surgery, the weight loss and
informed consent for the same. Patients were followed up at reduction in BMI were statistically significant in all the surgery
2 weeks, 1 month, 6 months, and 1 year postoperatively. Weight, groups.
BMI, excess weight loss, random blood sugar, systolic and diastolic On comparison of reduction in weight and BMI after 1 year of
blood pressure, and any complication following surgery were surgery between the different surgical groups, it was found that
documented at each visit. reduction in these parameters was more in LRYGB and LSG than
in LGI, and the difference is statistically significant (Tables 2 and 3).
Statistical Analysis Although the reduction in weight and BMI after 1 year of surgery
Paired t-test (two-tailed, dependent) has been used to find the was more in LRYGB than in LSG, the difference was not statistically
significance of study parameters on a continuous scale within each significant (Table 3).
group. Bonferroni and analysis of variance (ANOVA) have been used
to find the significance of study parameters between different dIscussIon
groups. For the analysis of the data, statistical software IBM SPSS
Statistics version 20.0 was used. The worldwide prevalence of obesity more than doubled between
5
P-value of less than 0.05 was considered statistically significant. 1980 and 2014. WHO estimated that in 2014, more than 1.9 billion
adults aged 18 years and older were overweight. Of these over 600
million adults were obese. Overall, about 13% of the world’s adult
results population (11% of men and 15% of women) were obese and 39%
Forty morbid obese patients were included in the study, of which 29 (38% of men and 40% of women) were overweight in 2014. 5
were females and 11 were males. Age varied from 19 to 50 years with Dietary therapy with exercise supplemented with
a mean of 37.75 years. Patients undergone LGI, LSG, and LRYGB had pharmacotherapy, with or without organization supervision,
a preoperative mean weight of 105.33 ± 8.87 kg, 104.07 ± 9.55 kg, generally achieved only minimal and often transient effects with
and 105.8 ± 9.52 kg, respectively; and a preoperative mean BMI of poor long-term results. Once severely obese, the likelihood that
−2
−2
−2
41.07 ± 2.51 kg m , 42.76 ± 3.81 kg m , and 43.27 ± 3.59 kg m , a person will lose enough weight by dietary means alone and
respectively (Fig. 1). remain at a BMI below 35 kg/m is estimated at 3% or less. The NIH
2
consensus conference recognized that for this patient population,
nonsurgical therapy has been uniformly unsuccessful in treating
the problem. 4
The rise in the prevalence of obesity led to increase interest
in the surgical approach to treat obesity, and in 1991, the NIH
established guidelines for surgical therapy of morbid obesity now
known as bariatric surgery. 2
A range of different bariatric procedures are available, working
on principles of restriction or malabsorption or both. Along with
reducing weight, some of them have been shown to reduce appetite
and improve glucose homeostasis independently of weight loss.
In view of its favorable metabolic effects, bariatric surgery is also
referred to as “metabolic surgery.”
6
Sleeve gastrectomy was initially described in 1988 by Hess
8
7
and Marceau during the duodenal switch and 1993 by Johnston
in an isolated form.
The gastric imbrication procedure involves plicating the greater
curvature of the stomach after the division of the short gastric
vessels. It is a relatively new technique. It was initially proposed by
Fig. 1: Graph showing preoperative and postoperative weight and BMI Wilkinson and Paleso 9,10 and introduced in 2006 by Dr. Talebpour in
Table 1: Analysis of weight and BMI reduction 1 year after surgery within a surgical group
LGI LSG LRYGB
−2
−2
−2
Weight (kg) BMI (kg m ) Weight (kg) BMI (kg m ) Weight (kg) BMI (kg m )
Preoperative; t = 0 105.33 ± 8.87 41.07 ± 2.51 104.07 ± 9.55 42.76 ± 3.81 105.8 ± 9.52 43.27 ± 3.59
Postoperative; t=1year 87.4 ± 6.58 34.08 ± 1.56 81.07 ± 6.32 33.32 ± 2.65 81.2 ± 7.04 33.18 ± 2.24
(Paired t-test) 0.000 0.000 0.000 0.000 0.000 0.000
P-value
World Journal of Laparoscopic Surgery, Volume 14 Issue 1 (January–April 2021) 27