Page 21 - WJOLS
P. 21
Comparison in Terms of Postoperative Morbidity and Hospital Stay between Open Cholecystectomy and LC
Since the introduction of laparoscopic cholecystectomy (LC) U Berggren and associates had noted that although laparos-
in 1987, numerous advances have been made in the technique. copic cholecystectomy has rapidly become established as the
LC has been shown to be safe for the emergency treatment of treatment of choice for cholelithiasis there is very little evidence
8
acute cholecystitis. In this era of increasing minimally invasive to support the claimed benefit to patients and they tried, with
surgery, conversion to open in cases of difficult dissection may success in their study to prove its effectiveness as in their
prove a difficult task for the exclusively laparoscopic surgeon. 9 study the mean duration of hospital stay and sick leave was
Age is one of the critical factors affecting the morbidity and significantly longer in patients who underwent open surgery
mortality rates after open cholecystectomy in both acute and for GS. Same results have been obtained in our study.
22
chronic cholecystitis (Table 1). 10, 11 Increasing age in patients J Wenner and his associates compared the financial aspects
undergoing open cholecystectomy has been associated with of both these procedures and reported a 10% lower hospital
12
increased length of hospital stay as well (Table 2). In a cost in patients who had laparoscopic surgery with lesser number
retrospective study by Jatzko GR, Lisbog PH and associates of days off work (14 versus 35 in open cholecystectomy)
age has been identified as the only significant factor in showing laparoscopic cholecystectomy to be more cost-effec-
increasing the morbidity rate after laparoscopic cholecystectomy 23
13
as well (Table 3). Julio Mayol and his associates have, tive. Although we did not compare the costs of these two
however, shown that Laparoscopic cholecystectomy is safe in procedures, the reduced hospital stay itself is an indicator of its
the aged (even above 70 years) for symptomatic gallbladder cost-effectivity (as patients spend lesser time and thus lesser
disease and is associated with a short hospital stay, low rates resources in the hospital and report back earlier to their jobs).
14
of readmissions and recurrent biliary surgery. Age has never However, Kory Jones and his associates argued that surgeons
been a contraindication for laparoscopic cholecystectomy, 15 should feel comfortable in converting from laparoscopic to open
although initially this approach was reserved for low-risk cholecystectomy in cases of tedious dissection as it does not
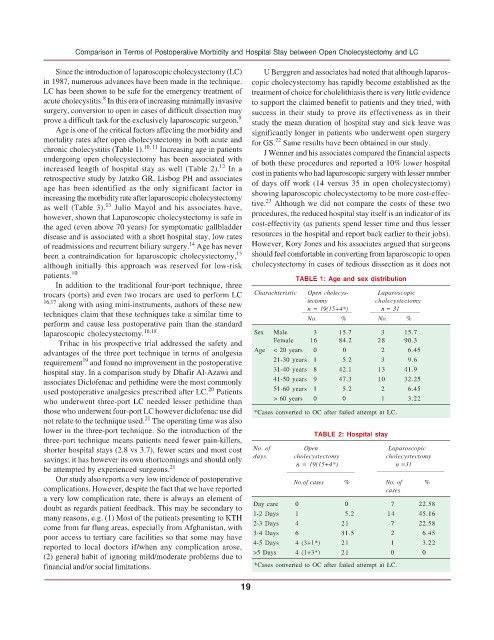
patients. 10 TABLE 1: Age and sex distribution
In addition to the traditional four-port technique, three
trocars (ports) and even two trocars are used to perform LC Charachteristic Open cholecys- Laparoscopic
16,17 along with using mini-instruments, authors of these new tectomy cholecystectomy
techniques claim that these techniques take a similar time to n = 19(15+4*) n = 31
perform and cause less postoperative pain than the standard No. % No. %
laparoscopic cholecystectomy. 16,18 Sex Male 3 15.7 3 15.7
Trihac in his prospective trial addressed the safety and Female 16 84.2 28 90.3
advantages of the three port technique in terms of analgesia Age < 20 years 0 0 2 6.45
19
requirement and found no improvement in the postoperative 21-30 years 1 5.2 3 9.6
hospital stay. In a comparison study by Dhafir Al-Azawi and 31-40 years 8 42.1 13 41.9
associates Diclofenac and pethidine were the most commonly 41-50 years 9 47.3 10 32.25
20
used postoperative analgesics prescribed after LC. Patients 51-60 years 1 5.2 2 6.45
who underwent three-port LC needed lesser pethidine than > 60 years 0 0 1 3.22
those who underwent four-port LC however diclofenac use did *Cases converted to OC after failed attempt at LC.
21
not relate to the technique used. The operating time was also
lower in the three-port technique. So the introduction of the TABLE 2: Hospital stay
three-port technique means patients need fewer pain-killers,
shorter hospital stays (2.8 vs 3.7), fewer scars and most cost No. of Open Laparoscopic
savings; it has however its own shortcomings and should only days cholecystectomy cholecystectomy
be attempted by experienced surgeons. 21 n = 19(15+4*) n =31
Our study also reports a very low incidence of postoperative No.of cases % No. of %
complications. However, despite the fact that we have reported cases
a very low complication rate, there is always an element of
doubt as regards patient feedback. This may be secondary to Day care 0 0 7 22.58
many reasons, e.g. (1) Most of the patients presenting to KTH 1-2 Days 1 5.2 14 45.16
come from far flung areas, especially from Afghanistan, with 2-3 Days 4 21 7 22.58
poor access to tertiary care facilities so that some may have 3-4 Days 6 31.5 2 6.45
reported to local doctors if/when any complication arose, 4-5 Days 4 (3+1*) 21 1 3.22
(2) general habit of ignoring mild/moderate problems due to >5 Days 4 (1+3*) 21 0 0
financial and/or social limitations. *Cases converted to OC after failed attempt at LC.
19