Page 24 - WJOLS - Laparoscopic Journal
P. 24
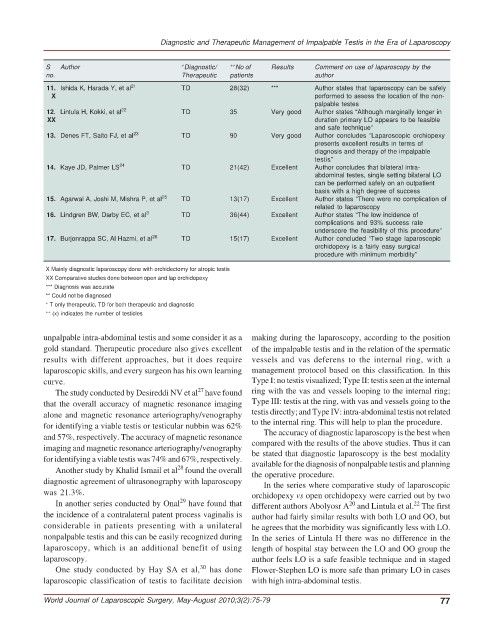
Diagnostic and Therapeutic Management of Impalpable Testis in the Era of Laparoscopy
S Author + Diagnostic/ ++ No of Results Comment on use of laparoscopy by the
no. Therapeutic patients author
11. Ishida K, Harada Y, et al 21 TD 28(32) *** Author states that laparoscopy can be safely
X performed to assess the location of the non-
palpable testes
12. Lintula H, Kokki, et al 22 TD 35 Very good Author states “Although marginally longer in
XX duration primary LO appears to be feasible
and safe technique”
13. Denes FT, Saito FJ, et al 23 TD 90 Very good Author concludes “Laparoscopic orchiopexy
presents excellent results in terms of
diagnosis and therapy of the impalpable
testis”
14. Kaye JD, Palmer LS 24 TD 21(42) Excellent Author concludes that bilateral intra-
abdominal testes, single setting bilateral LO
can be performed safely on an outpatient
basis with a high degree of success
15. Agarwal A, Joshi M, Mishra P, et al 25 TD 13(17) Excellent Author states “There were no complication of
related to laparoscopy
16. Lindgren BW, Darby EC, et al 3 TD 36(44) Excellent Author states “The low incidence of
complications and 93% success rate
underscore the feasibility of this procedure”
17. Burjonrappa SC, Al Hazmi, et al 26 TD 15(17) Excellent Author concluded “Two stage laparoscopic
orchidopexy is a fairly easy surgical
procedure with minimum morbidity”
X Mainly diagnostic laparoscopy done with orchidectomy for atropic testis
XX Comparative studies done between open and lap orchidopexy
*** Diagnosis was accurate
** Could not be diagnosed
+ T only therapeutic, TD for both therapeutic and diagnostic
++ (x) indicates the number of testicles
unpalpable intra-abdominal testis and some consider it as a making during the laparoscopy, according to the position
gold standard. Therapeutic procedure also gives excellent of the impalpable testis and in the relation of the spermatic
results with different approaches, but it does require vessels and vas deferens to the internal ring, with a
laparoscopic skills, and every surgeon has his own learning management protocol based on this classification. In this
curve. Type I: no testis visualized; Type II: testis seen at the internal
27
The study conducted by Desireddi NV et al have found ring with the vas and vessels looping to the internal ring;
that the overall accuracy of magnetic resonance imaging Type III: testis at the ring, with vas and vessels going to the
alone and magnetic resonance arteriography/venography testis directly; and Type IV: intra-abdominal testis not related
for identifying a viable testis or testicular nubbin was 62% to the internal ring. This will help to plan the procedure.
The accuracy of diagnostic laparoscopy is the best when
and 57%, respectively. The accuracy of magnetic resonance compared with the results of the above studies. Thus it can
imaging and magnetic resonance arteriography/venography be stated that diagnostic laparoscopy is the best modality
for identifying a viable testis was 74% and 67%, respectively. available for the diagnosis of nonpalpable testis and planning
28
Another study by Khalid Ismail et al found the overall the operative procedure.
diagnostic agreement of ultrasonography with laparoscopy In the series where comparative study of laparoscopic
was 21.3%. orchidopexy vs open orchidopexy were carried out by two
29
In another series conducted by Onal have found that different authors Abolyosr A and Lintula et al. The first
22
20
the incidence of a contralateral patent process vaginalis is author had fairly similar results with both LO and OO, but
considerable in patients presenting with a unilateral he agrees that the morbidity was significantly less with LO.
nonpalpable testis and this can be easily recognized during In the series of Lintula H there was no difference in the
laparoscopy, which is an additional benefit of using length of hospital stay between the LO and OO group the
laparoscopy. author feels LO is a safe feasible technique and in staged
30
One study conducted by Hay SA et al, has done Flower-Stephen LO is more safe than primary LO in cases
laparoscopic classification of testis to facilitate decision with high intra-abdominal testis.
World Journal of Laparoscopic Surgery, May-August 2010;3(2):75-79 77