Page 27 - WJOLS - Laparoscopic Journal
P. 27
WJOLS
Review of Literatures on Laparoscopic Prosthetic Repair of Giant Hiatal Hernia than Pure Anatomical Repair of Crura
REVIEW ARTICLE
Review of Literatures on Laparoscopic Prosthetic
Repair of Giant Hiatal Hernia than Pure Anatomical
Repair of Crura
Amol S Jeur
Registrar, Department of General Surgery, BMC Shri Bhagawati Hospital, Borivali (West), Mumbai, Maharashtra, India
Abstract
The recurrence rate after laparoscopic primary repair of giant hiatal hernias with paraesophageal involvement is reported to be high. Mesh
reinforcement repair of hiatal defect is proposed for solving this problem which is debated. The indication for mesh use, the type of mesh
to use, and the placement technique are controversial. After review of all literatures of our study it has been concluded that the use of
prosthetic reinforcement of cruroplasty in laparoscopic giant hiatal hernias has very low recurrence, though certain mesh related
complications are worse than recurrance which are up to certain extent are surgically correctable complications, as per different studies
no one mesh type is clearly superior in terms of avoiding failure and complication. Only further studies and long-term evaluation will allow
judgment of the effectiveness of laparoscopic mesh repair in patients with large hiatal hernias.
Keywords: Giant hiatal hernia, laparoscopic repair, prosthetic/mesh repair, nonabsorbable and reabsorbable/biological mesh, recurrence,
complications.
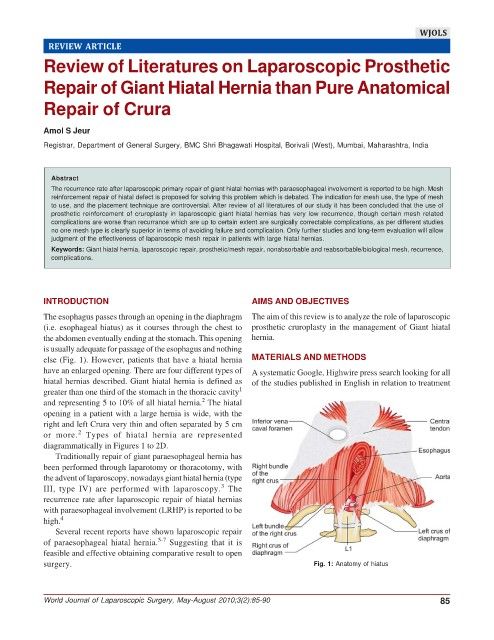
INTRODUCTION AIMS AND OBJECTIVES
The esophagus passes through an opening in the diaphragm The aim of this review is to analyze the role of laparoscopic
(i.e. esophageal hiatus) as it courses through the chest to prosthetic cruroplasty in the management of Giant hiatal
the abdomen eventually ending at the stomach. This opening hernia.
is usually adequate for passage of the esophagus and nothing
else (Fig. 1). However, patients that have a hiatal hernia MATERIALS AND METHODS
have an enlarged opening. There are four different types of A systematic Google, Highwire press search looking for all
hiatal hernias described. Giant hiatal hernia is defined as of the studies published in English in relation to treatment
greater than one third of the stomach in the thoracic cavity 1
2
and representing 5 to 10% of all hiatal hernia. The hiatal
opening in a patient with a large hernia is wide, with the
right and left Crura very thin and often separated by 5 cm
2
or more. Types of hiatal hernia are represented
diagrammatically in Figures 1 to 2D.
Traditionally repair of giant paraesophageal hernia has
been performed through laparotomy or thoracotomy, with
the advent of laparoscopy, nowadays giant hiatal hernia (type
3
III, type IV) are performed with laparoscopy. The
recurrence rate after laparoscopic repair of hiatal hernias
with paraesophageal involvement (LRHP) is reported to be
high. 4
Several recent reports have shown laparoscopic repair
5-7
of paraesophageal hiatal hernia. Suggesting that it is
feasible and effective obtaining comparative result to open
surgery. Fig. 1: Anatomy of hiatus
World Journal of Laparoscopic Surgery, May-August 2010;3(2):85-90 85