Page 26 - Journal of WALS
P. 26
WJOLS
Chronic Mesenteroaxial Gastric Volvulus and Congenital Diaphragmatic Hernia: Successful Laparoscopic Repair
freshened with diathermy. The defect was closed by
interrupted polyglactin 2/0 sutures using intracorporeal
knotting (Fig. 3). Chest tube was inserted under guidance
before taking the last two bites. The viscera were placed in
the normal anatomical position. Hemostasis was checked
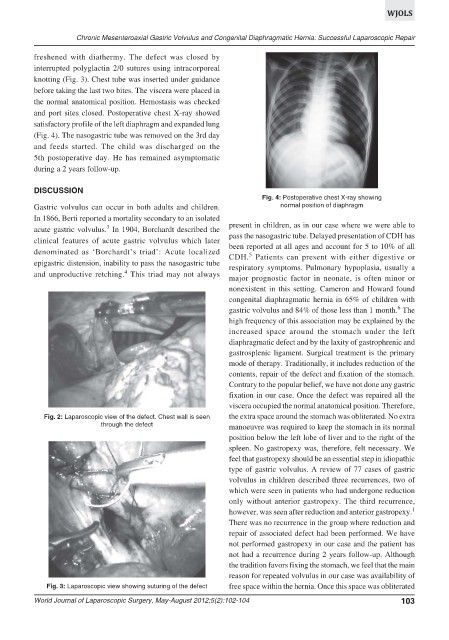
and port sites closed. Postoperative chest X-ray showed
satisfactory profile of the left diaphragm and expanded lung
(Fig. 4). The nasogastric tube was removed on the 3rd day
and feeds started. The child was discharged on the
5th postoperative day. He has remained asymptomatic
during a 2 years follow-up.
DISCUSSION
Fig. 4: Postoperative chest X-ray showing
Gastric volvulus can occur in both adults and children. normal position of diaphragm
In 1866, Berti reported a mortality secondary to an isolated
3
acute gastric volvulus. In 1904, Borchardt described the present in children, as in our case where we were able to
clinical features of acute gastric volvulus which later pass the nasogastric tube. Delayed presentation of CDH has
been reported at all ages and account for 5 to 10% of all
denominated as ‘Borchardt’s triad’: Acute localized
5
CDH. Patients can present with either digestive or
epigastric distension, inability to pass the nasogastric tube respiratory symptoms. Pulmonary hypoplasia, usually a
4
and unproductive retching. This triad may not always
major prognostic factor in neonate, is often minor or
nonexistent in this setting. Cameron and Howard found
congenital diaphragmatic hernia in 65% of children with
6
gastric volvulus and 84% of those less than 1 month. The
high frequency of this association may be explained by the
increased space around the stomach under the left
diaphragmatic defect and by the laxity of gastrophrenic and
gastrosplenic ligament. Surgical treatment is the primary
mode of therapy. Traditionally, it includes reduction of the
contents, repair of the defect and fixation of the stomach.
Contrary to the popular belief, we have not done any gastric
fixation in our case. Once the defect was repaired all the
viscera occupied the normal anatomical position. Therefore,
Fig. 2: Laparoscopic view of the defect. Chest wall is seen the extra space around the stomach was obliterated. No extra
through the defect manoeuvre was required to keep the stomach in its normal
position below the left lobe of liver and to the right of the
spleen. No gastropexy was, therefore, felt necessary. We
feel that gastropexy should be an essential step in idiopathic
type of gastric volvulus. A review of 77 cases of gastric
volvulus in children described three recurrences, two of
which were seen in patients who had undergone reduction
only without anterior gastropexy. The third recurrence,
however, was seen after reduction and anterior gastropexy. 1
There was no recurrence in the group where reduction and
repair of associated defect had been performed. We have
not performed gastropexy in our case and the patient has
not had a recurrence during 2 years follow-up. Although
the tradition favors fixing the stomach, we feel that the main
reason for repeated volvulus in our case was availability of
Fig. 3: Laparoscopic view showing suturing of the defect free space within the hernia. Once this space was obliterated
World Journal of Laparoscopic Surgery, May-August 2012;5(2):102-104 103