Page 22 - World Journal of Laparoscopic Surgery
P. 22
Salman Al-Sabah et al
for the antrum and blue cartridges for the body and 5 years, with the best results found in those with duration
fundus, aiming for a final gastric pouch size of 100 ml. of T2DM of 13 years (Table 2).
The calibrating bougie was then pulled proximally and Preoperatively, 2 patients were managed by pure
100 ml of methylene blue were injected through it to diet control, 68 were taking OHA, 15 were on insulin
assess for leak. No intrabdominal drains were placed. therapy, and 13 with a combination of insulin + OHA. In
Diabetes was defined in accordance with the Inter terms of treatment based outcomes, patients who were
national Diabetes Federation as a fasting blood glucose on diet control and OHA showed better remission of the
(FBG) level of more than 7.0 mmol/l, and HBA1C more disease than those on insulin and OHA + insulin (Table 3).
than 6.5%. The primary outcome measures were T2DM The difference between them however lacked statistical
resolution, defined as FBG of less than 7 mmol/l and significance.
HBA1C less than 6.5% in the absence of any hypoglycemic Median %EWL was 60% (10239) and was found to be
medications, and T2DM improvement, defined as a 72% at 1 year and 73% at 4 years (Graph 1). A significant
reduction in the dosage of hypoglycemic medications. association was found between the %EWL and complete
The resolution and improvement of diabetes were also remission compared to just improvement of T2DM (Graph 2).
grouped and analyzed in terms of time since T2DM The median postoperative BMI was 33 kg/m (2061).
2
onset and treatment type: diet, oral hypoglycemic agents
(OHA), insulin, and insulin + OHA. Secondary outcomes DiSCuSSion
measures included change in FBG and HBA1C levels pre
and postoperative, percent excess weight loss (%EWL), The findings of this study clearly point to the fact that
and change in BMI. LSG can play a significant role in managing T2DM. The
The study was approved by the Kuwait Institute for fact that the vast majority (91.6%) of patients showed either
Medical Specialization and Kuwait Ministry of Health complete remission or improvement of the disease is in
ethical committees. Statistical analysis of the data was keeping with the emerging literature focusing on LSG as
carried out using SPSS software. Statistical significance a potential option for the management of diabetes. Most
was calculated using Fisher’s exact test and was set at a current studies comprise of a substantially small patient
pvalue less than 0.05. population but show significant improvement in blood
glucose levels, almost reaching near normal figures in
RESuLTS known T2DM.
In a 2010 systemic review of 27 studies with 673 patients,
The data from a total of 1,202 patients who underwent
LSG at AlAmiri Hospital was retrieved and analyzed. LSG was shown to resolve diabetes in 66.2% of the
A total of 185 (15.4%) patients were found to be diabetic, subjects, with 97.1% experiencing resolution or improve
6
107 of whom had the required laboratory investigations ment. The drop in baseline FBG (11 mmol/l to 6 mmol/l)
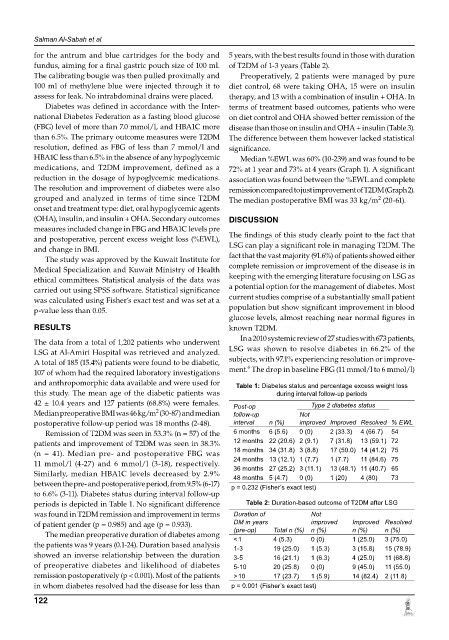
and anthropomorphic data available and were used for Table 1: Diabetes status and percentage excess weight loss
this study. The mean age of the diabetic patients was during interval follow-up periods
42 ± 10.4 years and 127 patients (68.8%) were females. Post-op Type 2 diabetes status
2
Median preoperative BMI was 46 kg/m (3087) and median follow-up Not
postoperative followup period was 18 months (248). interval n (%) improved Improved Resolved % EWL
Remission of T2DM was seen in 53.3% (n = 57) of the 6 months 6 (5.6) 0 (0) 2 (33.3) 4 (66.7) 54
patients and improvement of T2DM was seen in 38.3% 12 months 22 (20.6) 2 (9.1) 7 (31.8) 13 (59.1) 72
(n = 41). Median pre and postoperative FBG was 18 months 34 (31.8) 3 (8.8) 17 (50.0) 14 (41.2) 75
11 mmol/l (427) and 6 mmol/l (318), respectively. 24 months 13 (12.1) 1 (7.7) 1 (7.7) 11 (84.6) 75
Similarly, median HBA1C levels decreased by 2.9% 36 months 27 (25.2) 3 (11.1) 13 (48.1) 11 (40.7) 65
1 (20)
73
0 (0)
48 months 5 (4.7)
4 (80)
between the pre and postoperative period, from 9.5% (617) p = 0.232 (Fisher’s exact test)
to 6.6% (311). Diabetes status during interval followup
periods is depicted in Table 1. No significant difference Table 2: Duration-based outcome of T2DM after LSG
was found in T2DM remission and improvement in terms Duration of Not
of patient gender (p = 0.985) and age (p = 0.933). DM in years improved Improved Resolved
The median preoperative duration of diabetes among (pre-op) Total n (%) n (%) n (%) n (%)
1 (25.0)
0 (0)
4 (5.3)
3 (75.0)
< 1
the patients was 9 years (0.124). Duration based analysis 1-3 19 (25.0) 1 (5.3) 3 (15.8) 15 (78.9)
showed an inverse relationship between the duration 3-5 16 (21.1) 1 (6.3) 4 (25.0) 11 (68.8)
of preoperative diabetes and likelihood of diabetes 5-10 20 (25.8) 0 (0) 9 (45.0) 11 (55.0)
remission postoperatively (p < 0.001). Most of the patients > 10 17 (23.7) 1 (5.9) 14 (82.4) 2 (11.8)
in whom diabetes resolved had the disease for less than p = 0.001 (Fisher’s exact test)
122