Page 26 - World Journal of Laparoscopic Surgery
P. 26
Abid Ali Karatparambil, C Sidhic
was done (specialized laparoscopic bariatric institution
were given the preference).
PATIEnT SELECTIOn
A history of obesity of > 5 years’ duration; BMI > 40 kg/m 2
2
or BMI > 35 kg/m with comorbidities; documented
weight loss attempts in the past; and good motivation
for surgery. The age was restricted to patients from 18 to
59 years of age. Exclusion criteria were previous obesity
surgery, previous gastric surgery, large abdominal ventral
2
hernia, pregnancy, psychiatric illness, or BMI > 60 kg/m .
OPERATIVE TECHnIQuES
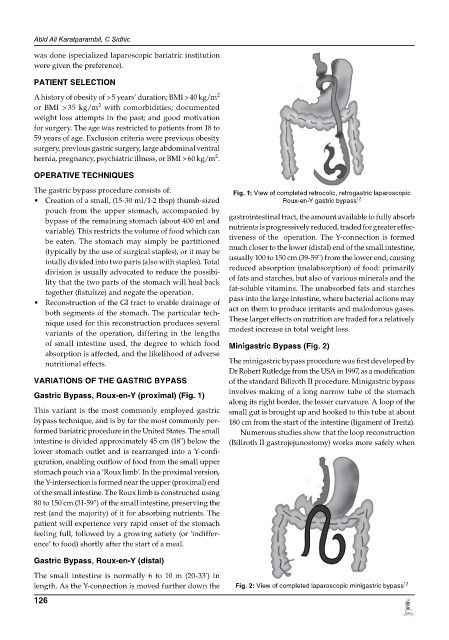
The gastric bypass procedure consists of: Fig. 1: View of completed retrocolic, retrogastric laparoscopic
• Creation of a small, (15-30 ml/1-2 tbsp) thumb-sized Roux-en-Y gastric bypass 12
pouch from the upper stomach, accompanied by
bypass of the remaining stomach (about 400 ml and gastrointestinal tract, the amount available to fully absorb
variable). This restricts the volume of food which can nutrients is progressively reduced, traded for greater effec-
be eaten. The stomach may simply be partitioned tiveness of the operation. The Y-connection is formed
(typically by the use of surgical staples), or it may be much closer to the lower (distal) end of the small intestine,
totally divided into two parts (also with staples). Total usually 100 to 150 cm (39-59'') from the lower end, causing
division is usually advocated to reduce the possibi- reduced absorption (malabsorption) of food: primarily
lity that the two parts of the stomach will heal back of fats and starches, but also of various minerals and the
together (fistulize) and negate the operation. fat-soluble vitamins. The unabsorbed fats and starches
• Reconstruction of the GI tract to enable drainage of pass into the large intestine, where bacterial actions may
both segments of the stomach. The particular tech- act on them to produce irritants and malodorous gases.
nique used for this reconstruction produces several These larger effects on nutrition are traded for a relatively
variants of the operation, differing in the lengths modest increase in total weight loss.
of small intestine used, the degree to which food Minigastric Bypass (fig. 2)
absorption is affected, and the likelihood of adverse
nutritional effects. The minigastric bypass procedure was first developed by
Dr Robert Rutledge from the USA in 1997, as a modification
VARIATIOnS Of THE gASTRIC BYPASS of the standard Billroth II procedure. Minigastric bypass
gastric Bypass, Roux-en-Y (proximal) (fig. 1) involves making of a long narrow tube of the stomach
along its right border, the lesser curvature. A loop of the
This variant is the most commonly employed gastric small gut is brought up and hooked to this tube at about
bypass technique, and is by far the most commonly per- 180 cm from the start of the intestine (ligament of Treitz).
formed baria tric procedure in the United States. The small Numerous studies show that the loop reconstruction
intestine is divided approximately 45 cm (18'') below the (Billroth II gastrojejunostomy) works more safely when
lower stomach outlet and is rearranged into a Y-confi-
guration, enabling outflow of food from the small upper
stomach pouch via a ‘Roux limb’. In the proximal version,
the Y-intersection is formed near the upper (proximal) end
of the small intestine. The Roux limb is constructed using
80 to 150 cm (31-59'') of the small intestine, preserving the
rest (and the majority) of it for absorbing nutrients. The
patient will experience very rapid onset of the stomach
feeling full, followed by a growing satiety (or ‘indiffer-
ence’ to food) shortly after the start of a meal.
gastric Bypass, Roux-en-Y (distal)
The small intestine is normally 6 to 10 m (20-33') in
length. As the Y-connection is moved further down the Fig. 2: View of completed laparoscopic minigastric bypass 12
126