Page 31 - WJOLS - Laparoscopic Journal
P. 31
WJOLS
Role of Minimally Invasive Surgery in Gynecological Cancers
evaluated the feasibility and safety of pretreatment malignancy according to FIGO. The importance of pelvic
laparoscopic surgical staging in the treatment of locally and para-aortic lymph node status documented by a large
advanced cervical cancer. The authors contended that GOG study was instrumental in motivating the change
pretreatment laparoscopy is the best guideline for indi- to surgical staging.
vidualized concurrent chemoradiation. When compared Various studies are summarized in Table 2:
with magnetic resonance imaging, laparoscopic surgical Patients managed with a laparoscopic approach had
staging was superior in detecting microscopic lymph the same number of lymph nodes removed, but had less
node metastases. complications, a shorter hospital stay and quicker recovery
Various studies summarized in Tables 1 to 3 respec- than the laparotomy group. In addition to surgical staging
tively at various places. in the primary management of endometrial carcinoma
Thus, while abdominal radical hysterectomy remains patients, the technique can be utilized in patients with
the standard of care for early-stage cervical cancer, lapa- incomplete staging of disease at their primary surgery.
roscopic radical hysterectomy appears to be a safe, rea-
sonable alternative. Operative laparoscopy has also been Ovarian Cancers
used as a means of determining a patient’s eligibility for Epithelial ovarian cancer is one of the leading causes of
pelvic exenteration for recurrent cervical cancer, removal death in gynecological malignancies and the seventh
of diseased adnexae, and ovarian transposition. It has most common cancer in the world among women. Mini-
been proven to be a valuable step in the workup and man- mally invasive surgery for patients with ovarian cancer
agement of patients with locally recurrent cervical cancer. can be incorporated in different ways depending on the
stage of disease and surgical goals of the procedure. In
Endometrial Cancer
advanced stage disease, laparoscopy in general can be
Operative laparoscopy is also useful in the management used to confirm diagnosis and determine resectability.
of patients with malignancies of the uterine corpus. In In early-stage disease, patients can be comprehensively
1988, endometrial cancer became a surgically staged staged via the laparoscopic approach. The laparoscopic
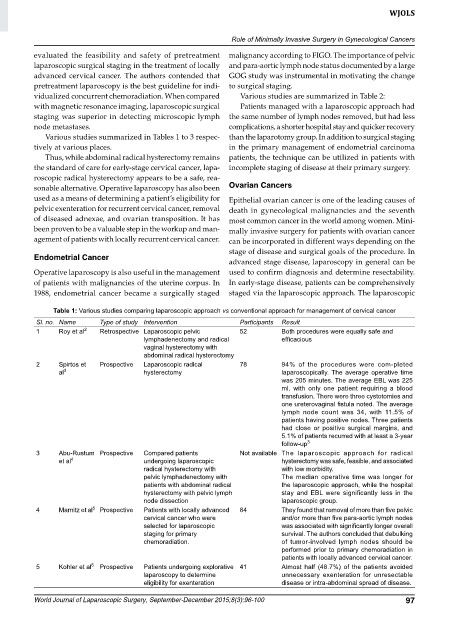
Table 1: Various studies comparing laparoscopic approach vs conventional approach for management of cervical cancer
Sl. no. Name Type of study Intervention Participants Result
1 Roy et al 2 Retrospective Laparoscopic pelvic 52 Both procedures were equally safe and
lymphadenectomy and radical efficacious
vaginal hysterectomy with
abdominal radical hysterectomy
2 Spirtos et Prospective Laparoscopic radical 78 94% of the procedures were com-pleted
al 3 hysterectomy laparoscopically. The average operative time
was 205 minutes. The average EBL was 225
ml, with only one patient requiring a blood
transfusion. There were three cystotomies and
one ureterovaginal fistula noted. The average
lymph node count was 34, with 11.5% of
patients having positive nodes. Three patients
had close or positive surgical margins, and
5.1% of patients recurred with at least a 3-year
follow-up 3
3 Abu-Rustum Prospective Compared patients Not available The laparoscopic approach for radical
et al 4 undergoing laparoscopic hysterectomy was safe, feasible, and associated
radical hysterectomy with with low morbidity.
pelvic lymphadenectomy with The median operative time was longer for
patients with abdominal radical the laparoscopic approach, while the hospital
hysterectomy with pelvic lymph stay and EBL were significantly less in the
node dissection laparoscopic group.
4 Marnitz et al 5 Prospective Patients with locally advanced 84 They found that removal of more than five pelvic
cervical cancer who were and/or more than five para-aortic lymph nodes
selected for laparoscopic was associated with signifi cantly longer overall
staging for primary survival. The authors concluded that debulking
chemoradiation. of tumor-involved lymph nodes should be
performed prior to primary chemoradiation in
patients with locally advanced cervical cancer.
5 Kohler et al 6 Prospective Patients undergoing explorative 41 Almost half (48.7%) of the patients avoided
laparoscopy to determine unnecessary exenteration for unresectable
eligibility for exenteration disease or intra-abdominal spread of disease.
World Journal of Laparoscopic Surgery, September-December 2015;8(3):96-100 97