Page 32 - WJOLS - Laparoscopic Journal
P. 32
Rajendra Shitole
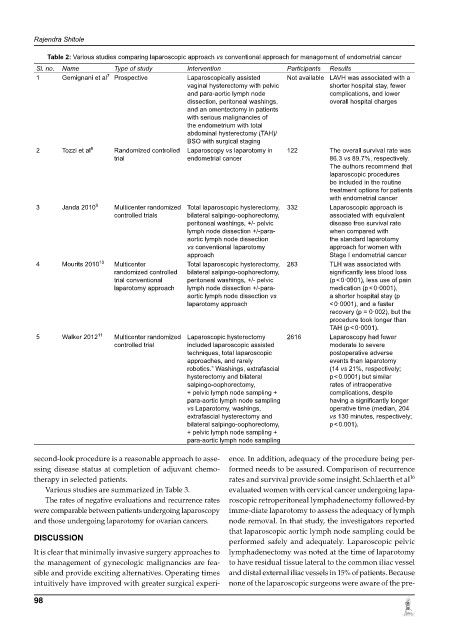
Table 2: Various studies comparing laparoscopic approach vs conventional approach for management of endometrial cancer
Sl. no. Name Type of study Intervention Participants Results
1 Gemignani et al 7 Prospective Laparoscopically assisted Not available LAVH was associated with a
vaginal hysterectomy with pelvic shorter hospital stay, fewer
and para-aortic lymph node complications, and lower
dissection, peritoneal washings, overall hospital charges
and an omentectomy in patients
with serious malignancies of
the endometrium with total
abdominal hysterectomy (TAH)/
BSO with surgical staging
2 Tozzi et al 8 Randomized controlled Laparoscopy vs laparotomy in 122 The overall survival rate was
trial endometrial cancer 86.3 vs 89.7%, respectively.
The authors recommend that
laparoscopic procedures
be included in the routine
treatment options for patients
with endometrial cancer
3 Janda 2010 9 Multicenter randomized Total laparoscopic hysterectomy, 332 Laparoscopic approach is
controlled trials bilateral salpingo-oophorectomy, associated with equivalent
peritoneal washings, +/- pelvic disease free survival rate
lymph node dissection +/-para- when compared with
aortic lymph node dissection the standard laparotomy
vs conventional laparotomy approach for women with
approach Stage I endometrial cancer
4 Mourits 2010 10 Multicenter Total laparoscopic hysterectomy, 283 TLH was associated with
randomized controlled bilateral salpingo-oophorectomy, significantly less blood loss
trial conventional peritoneal washings, +/- pelvic (p < 0·0001), less use of pain
laparotomy approach lymph node dissection +/-para- medication (p < 0·0001),
aortic lymph node dissection vs a shorter hospital stay (p
laparotomy approach < 0·0001), and a faster
recovery (p = 0·002), but the
procedure took longer than
TAH (p < 0·0001).
5 Walker 2012 11 Multicenter randomized Laparoscopic hysterectomy 2616 Laparoscopy had fewer
controlled trial included laparoscopic assisted moderate to severe
techniques, total laparoscopic postoperative adverse
approaches, and rarely events than laparotomy
robotics.” Washings, extrafascial (14 vs 21%, respectively;
hysterectomy and bilateral p < 0.0001) but similar
salpingo-oophorectomy, rates of intraoperative
+ pelvic lymph node sampling + complications, despite
para-aortic lymph node sampling having a significantly longer
vs Laparotomy, washings, operative time (median, 204
extrafascial hysterectomy and vs 130 minutes, respectively;
bilateral salpingo-oophorectomy, p < 0.001).
+ pelvic lymph node sampling +
para-aortic lymph node sampling
second-look procedure is a reasonable approach to asse- ence. In addition, adequacy of the procedure being per-
ssing disease status at completion of adjuvant chemo- formed needs to be assured. Comparison of recurrence
16
therapy in selected patients. rates and survival provide some insight. Schlaerth et al
Various studies are summarized in Table 3. evaluated women with cervical cancer undergoing lapa-
The rates of negative evaluations and recurrence rates roscopic retroperitoneal lymphadenectomy followed-by
were comparable between patients undergoing laparoscopy imme-diate laparotomy to assess the adequacy of lymph
and those undergoing laparotomy for ovarian cancers. node removal. In that study, the investigators reported
that laparoscopic aortic lymph node sampling could be
DISCUSSION
performed safely and adequately. Laparoscopic pelvic
It is clear that minimally invasive surgery approaches to lymphadenectomy was noted at the time of laparotomy
the management of gynecologic malignancies are fea- to have residual tissue lateral to the common iliac vessel
sible and provide exciting alternatives. Operating times and distal external iliac vessels in 15% of patients. Because
intuitively have improved with greater surgical experi- none of the laparoscopic surgeons were aware of the pre-
98