Page 27 - Journal of Laparoscopic Surgery
P. 27
WJOLS
Laparoscopic versus open Varicocelectomy: An Observational Study
6
Table 3: Duration of surgery was 5%. Similarly, Gouda El-labban reported significant
improvement in semen parameters in both laparoscopic
Laparoscopic (Group B) 48 minutes (mean)
Open (Group A) 57 minutes (mean) and open groups. Al-Kandari et al. found that improve-
ment in sperm motility and/or concentration was com-
the postoperative analgesic requirement was almost parable and observed in 65%, 67%, and 76% of the open,
equal to available series in the literature recurrence was laparoscopic, and micro-surgical groups, respectively.
observed in one patient during the follow-up period. Also, the pregnancy rate at 1 year was not significantly
13
Shamsa et al. reported recurrence in 2 (6.7%) patients of different and was 28%, 30%, and 40% in the three groups
the laparoscopic group, but it was not observed in patients respectively. 16
who underwent open varicocelectomy. Watanabe et al. We observed that in the laparoscopic group an
reported 6.1% recurrence in 33 patients with bilateral average hospital stay of 35.6 hours which was sig-
laparoscopic varicocelectomy. They mentioned a recur- nificantly less than the open surgical group with an
rence rate of 12% in 50 patients with unilateral varicoce- average hospital stay of 50.6 hours (Graph 4 and Table 7).
6
lectomy by high retroperitoneal method. 14 Gouda El-labban in his comparative study observed
The hydrocele is another complication of varicoce- that patients in open varicocelectomy stayed in the hos-
lectomy (Graph 3, Table 4). The incidence of this com- pital much longer than the laparoscopic group with an
15
plication is 0.3% to 40.4% as reported by Kočvara et al. average of 3 days versus 1.5 days respectively. Osman
Etiology of post varicocelectomy hydrocele is ligation of et al. reported that the postoperative hospital stay
the lymphatic vessels that are colorless and sometimes was 52 hours and 8.4 hours in open and laparoscopic
17
are mistaken for veins. 16 varicocelectomy group respectively. Podkamenev et
The improvement in the quality of semen was ana- al. reported average hospital stay of 3 days for lapa-
lyzed and compared with the pre-operative semen analy- roscopic varicocelectomy versus 7 days for open vari-
18
sis (Tables 5 and 6). Preoperative semen analysis was done cocelectomy. Similarly, Bebars et al. observed longer
1 week before surgery, and then postoperative semen postoperative hospital stay in open as compared to
analysis was advised 3 months after varicocelectomy. laparoscopic varicocelectomy group and it was 3.5 (2-8)
7
In the present series, we found that the mean improve- days versus 1.3 (1-3) days. Ogura et al. also observed
ment in sperm concentration was 8.9 million/mL. The the shorter length of hospital stay for the laparoscopic
mean percentage of improvement in sperm motility was patients than for the open surgery group (0.97 vs 1.42
19
approx. 5.5%. The average decrease in abnormal forms days, p = 0.0078). Zain H Al-Sharief et al. in their
series reported hospital stay of 2 days versus 5 days in
Table 4: Varicocelectomy complications with laparoscopic varicocelectomy and open varicocelectomy,
different surgical methods
Laparoscopic
Complication (number of patients) C
Pain 6 11
Hydrocele 5 3
Scrotal edema 1 1
Orchitis 2 2
Wound infection 0 6
Recurrence 3 1
Table 5: Semen analysis results with
different varicocelectomy methods
Laparoscopic
Varicocelectomy Before treatment After treatment
Sperm count × 106/ml 52 ± 36 44 ± 30
Sperm motility % 70 ± 50 88 ± 80
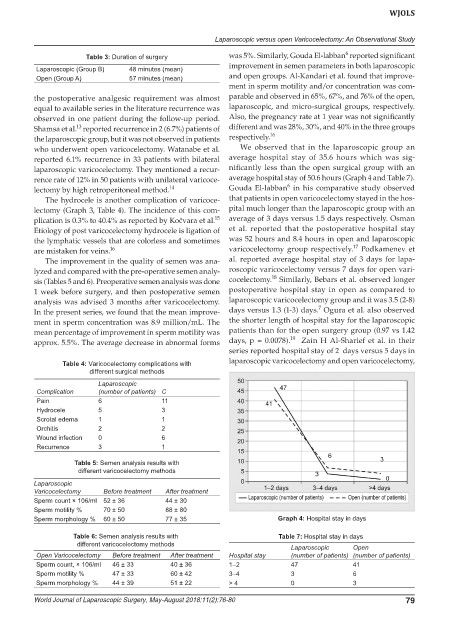
Sperm morphology % 60 ± 50 77 ± 35 Graph 4: Hospital stay in days
Table 6: Semen analysis results with Table 7: Hospital stay in days
different varicocelectomy methods
Laparoscopic Open
Open Varicocelectomy Before treatment After treatment Hospital stay (number of patients) (number of patients)
Sperm count, × 106/ml 46 ± 33 40 ± 36 1–2 47 41
Sperm motility % 47 ± 33 60 ± 42 3–4 3 6
Sperm morphology % 44 ± 39 51 ± 22 > 4 0 3
World Journal of Laparoscopic Surgery, May-August 2018;11(2):76-80 79