Page 25 - Journal of Laparoscopic Surgery
P. 25
WJOLS
Laparoscopic versus open Varicocelectomy: An Observational Study
in Group A and 10 years to 36 years (average 23 years) in from the veins. Then, the veins were ligated by clips or by
group B. Majority of patients presented with complaints intracorporeal knotting. After verifying the hemostasis,
of swelling in the left hemiscrotum, detected incidentally. trocars were removed and incision sutured. Antiseptic
Dragging sensation in the scrotal region was the second laparoscopic dressings were applied.
most common complaint. Few of the patients who were
above 25 years of age presented with primary or second- Open Surgery
ary infertility. The diagnosis was established mainly by Open high ligation of testicular veins was done under
clinical examination and scrotal ultrasound. Majority spinal or general anesthesia. A small muscle splitting
of patients had a unilateral varicocele (77% in Group A incision made at the level of the anterior superior iliac
and 79% in Group B). The diagnosis was confirmed by spine, and the retroperitoneal space was entered, with
Doppler in all cases. Semen analysis was performed in the peritoneal envelope swept medially to identify the
patients presenting with infertility at least twice preoper- internal spermatic vessels. These vessels were ligated
atively and every 6 months postoperatively for 18 months. and divided. Great care was taken to preserve testicular
artery. The external spermatic fascia was sutured, and
SURGICAL TECHNIQUE the wound was closed in layers. The antiseptic dressing
Laparoscopic Varicocelectomy was applied.
Patients were operated in supine position under general AIM AND OBJECTIVES
anesthesia. A urinary catheter was inserted after the induc-
tion of anesthesia to evacuate the bladder or the patient was To compare the outcome of laparoscopic with open vari-
asked to void just before shifting to the operation room. Post cocelectomy in terms of;
induction nasogastric tube was passed to decompress the • Operative time.
stomach. A veress needle for the creation of pneumoperi- • Complications.
toneum was introduced through a small infra-umbilical • Improvement in semen analysis after 3 months.
incision. Then, the abdomen was inflated with CO gas, the • Analgesic requirement.
2
pressure maintained between 12–14 mm Hg. The head end • Hospital stay.
of the bed was lowered 150 to 300 to displace the bowel away
from the lower quadrants of the abdomen. Veress needle RESULTS
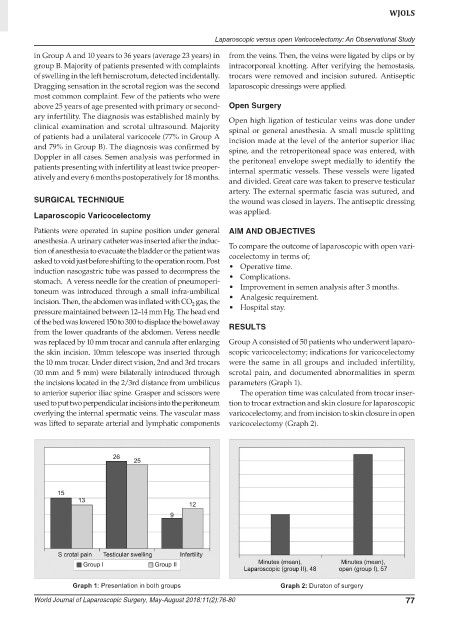
was replaced by 10 mm trocar and cannula after enlarging Group A consisted of 50 patients who underwent laparo-
the skin incision. 10mm telescope was inserted through scopic varicocelectomy; indications for varicocelectomy
the 10 mm trocar. Under direct vision, 2nd and 3rd trocars were the same in all groups and included infertility,
(10 mm and 5 mm) were bilaterally introduced through scrotal pain, and documented abnormalities in sperm
the incisions located in the 2/3rd distance from umbilicus parameters (Graph 1).
to anterior superior iliac spine. Grasper and scissors were The operation time was calculated from trocar inser-
used to put two perpendicular incisions into the peritoneum tion to trocar extraction and skin closure for laparoscopic
overlying the internal spermatic veins. The vascular mass varicocelectomy, and from incision to skin closure in open
was lifted to separate arterial and lymphatic components varicocelectomy (Graph 2).
Graph 1: Presentation in both groups Graph 2: Duraton of surgery
World Journal of Laparoscopic Surgery, May-August 2018;11(2):76-80 77