Page 21 - WJOLS - World Journal of Laparoscopic Surgery
P. 21
Safety and Efficacy of Laparoscopic Appendectomy in Pregnancy
Table 1: Preoperative demographic and clinical data
Perioperative data LA (18 patients) OA (13 patients) p value
Age 18–29 (26 ± 2.8) 23–35 (29.2 ± 3.2) 0.7*
years years
BMI 23.4 ± 3.1 23.1 ± 2.8 0.366*
Gestation age at 18.4 ± 6.2 weeks 18.6 ± 5.4 weeks 0.317*
operation
1st trimester 4 (22.22%) 3 (23.08%) 0.342**
2nd trimester 11 (61.11%) 5 (38.46%)
3rd trimester 3 (16.67%) 5 (38.46%)
Previous CS 4 (22.22%) 7 (53.85%) 0.069**
Preoperative U/S 18 (100%) 13 (100%) 0.764**
False-positive 2 (11.11%) 3 (23.08%)
False-negative 2 (11.11%) 2 (15.38%)
*t test p value
**Chi-square test p value
Table 2: The final histopathological diagnosis after operation
2
LA (18 OA (13 Χ
Trimester Final histopathology patients) patients) p value
1st trimester Normal appendix 0 0 1
Acute suppurative 3 2
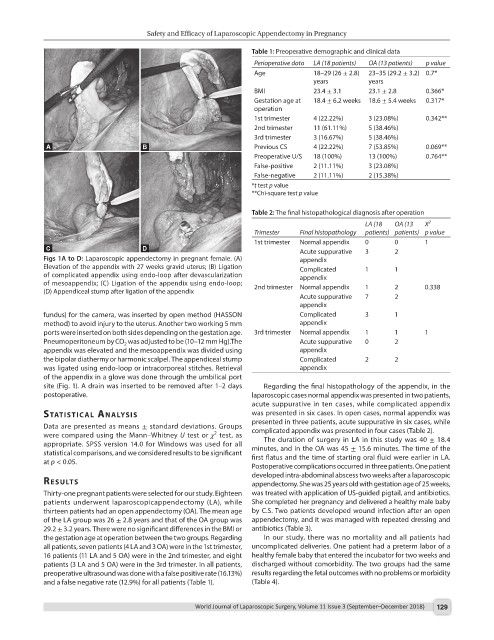
Figs 1A to D: Laparoscopic appendectomy in pregnant female. (A) appendix
Elevation of the appendix with 27 weeks gravid uterus; (B) Ligation Complicated 1 1
of complicated appendix using endo-loop after devascularization appendix
of mesoappendix; (C) Ligation of the appendix using endo-loop; 2nd trimester Normal appendix 1 2 0.338
(D) Appendiceal stump after ligation of the appendix
Acute suppurative 7 2
appendix
fundus) for the camera, was inserted by open method (HASSON Complicated 3 1
method) to avoid injury to the uterus. Another two working 5 mm appendix
ports were inserted on both sides depending on the gestation age. 3rd trimester Normal appendix 1 1 1
Pneumoperitoneum by CO was adjusted to be (10–12 mm Hg).The Acute suppurative 0 2
2
appendix was elevated and the mesoappendix was divided using appendix
the bipolar diathermy or harmonic scalpel. The appendiceal stump Complicated 2 2
was ligated using endo-loop or intracorporeal stitches. Retrieval appendix
of the appendix in a glove was done through the umbilical port
site (Fig. 1). A drain was inserted to be removed after 1–2 days Regarding the final histopathology of the appendix, in the
postoperative. laparoscopic cases normal appendix was presented in two patients,
acute suppurative in ten cases, while complicated appendix
stAtIstIcAl AnAlysIs was presented in six cases. In open cases, normal appendix was
presented in three patients, acute suppurative in six cases, while
Data are presented as means ± standard deviations. Groups complicated appendix was presented in four cases (Table 2).
2
were compared using the Mann–Whitney U test or χ test, as The duration of surgery in LA in this study was 40 ± 18.4
appropriate. SPSS version 14.0 for Windows was used for all minutes, and in the OA was 45 ± 15.6 minutes. The time of the
statistical comparisons, and we considered results to be significant first flatus and the time of starting oral fluid were earlier in LA.
at p < 0.05.
Postoperative complications occurred in three patients. One patient
developed intra-abdominal abscess two weeks after a laparoscopic
results appendectomy. She was 25 years old with gestation age of 25 weeks,
Thirty-one pregnant patients were selected for our study. Eighteen was treated with application of US-guided pigtail, and antibiotics.
patients underwent laparoscopicappendectomy (LA), while She completed her pregnancy and delivered a healthy male baby
thirteen patients had an open appendectomy (OA). The mean age by C.S. Two patients developed wound infection after an open
of the LA group was 26 ± 2.8 years and that of the OA group was appendectomy, and it was managed with repeated dressing and
29.2 ± 3.2 years. There were no significant differences in the BMI or antibiotics (Table 3).
the gestation age at operation between the two groups. Regarding In our study, there was no mortality and all patients had
all patients, seven patients (4 LA and 3 OA) were in the 1st trimester, uncomplicated deliveries. One patient had a preterm labor of a
16 patients (11 LA and 5 OA) were in the 2nd trimester, and eight healthy female baby that entered the incubator for two weeks and
patients (3 LA and 5 OA) were in the 3rd trimester. In all patients, discharged without comorbidity. The two groups had the same
preoperative ultrasound was done with a false positive rate (16.13%) results regarding the fetal outcomes with no problems or morbidity
and a false negative rate (12.9%) for all patients (Table 1). (Table 4).
World Journal of Laparoscopic Surgery, Volume 11 Issue 3 (September–December 2018) 129