Page 25 - WJOLS - World Journal of Laparoscopic Surgery
P. 25
Laparoscopic Cholecystectomy in Gombe, Nigeria
9
also seen in a report by Afuwape et al. The duration of LC was
73 (±17.4) minutes while OC was 92 (±28.0) minutes and was
not statistically significant. The duration of LC was longer than
14
47 minutes recorded by Salam et al. The prolonged duration
was due to the learning curve and some technical issues, such as
instrument malfunction and unstable power supply. However, it
7,10
is comparable to other studies. The mean length of hospital
stay for LC was 5.8 (±5.5) days while for OC it was 10 (±8.5) days.
7,10,15
This was longer than those seen in other studies but shorter
9
than 7.5 days seen in Afuwape et al. Some centers perform LC as
6,16
a day-case. Being a new procedure, we were cautious to avoid
rejection, hence the long duration of hospital stay.
All patients had paracetamol and pentazocine injections
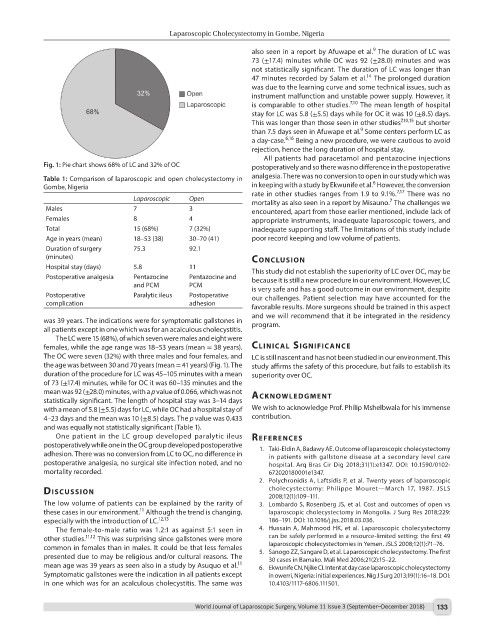
Fig. 1: Pie chart shows 68% of LC and 32% of OC postoperatively and so there was no difference in the postoperative
Table 1: Comparison of laparoscopic and open cholecystectomy in analgesia. There was no conversion to open in our study which was
6
Gombe, Nigeria in keeping with a study by Ekwunife et al. However, the conversion
7,17
rate in other studies ranges from 1.9 to 9.1%. There was no
Laparoscopic Open mortality as also seen in a report by Misauno. The challenges we
7
Males 7 3 encountered, apart from those earlier mentioned, include lack of
Females 8 4 appropriate instruments, inadequate laparoscopic towers, and
Total 15 (68%) 7 (32%) inadequate supporting staff. The limitations of this study include
Age in years (mean) 18–53 (38) 30–70 (41) poor record keeping and low volume of patients.
Duration of surgery 75.3 92.1
(minutes) conclusIon
Hospital stay (days) 5.8 11 This study did not establish the superiority of LC over OC, may be
Postoperative analgesia Pentazocine Pentazocine and because it is still a new procedure in our environment. However, LC
and PCM PCM is very safe and has a good outcome in our environment, despite
Postoperative Paralytic ileus Postoperative our challenges. Patient selection may have accounted for the
complication adhesion
favorable results. More surgeons should be trained in this aspect
and we will recommend that it be integrated in the residency
was 39 years. The indications were for symptomatic gallstones in program.
all patients except in one which was for an acalculous cholecystitis.
The LC were 15 (68%), of which seven were males and eight were
females, while the age range was 18–53 years (mean = 38 years). clInIcAl sIgnIfIcAnce
The OC were seven (32%) with three males and four females, and LC is still nascent and has not been studied in our environment. This
the age was between 30 and 70 years (mean = 41 years) (Fig. 1). The study affirms the safety of this procedure, but fails to establish its
duration of the procedure for LC was 45–105 minutes with a mean superiority over OC.
of 73 (±17.4) minutes, while for OC it was 60–135 minutes and the
mean was 92 (±28.0) minutes, with a p value of 0.066, which was not AcknowledgMent
statistically significant. The length of hospital stay was 3–14 days
with a mean of 5.8 (±5.5) days for LC, while OC had a hospital stay of We wish to acknowledge Prof. Philip Mshelbwala for his immense
4–23 days and the mean was 10 (±8.5) days. The p value was 0.433 contribution.
and was equally not statistically significant (Table 1).
One patient in the LC group developed paralytic ileus references
postoperatively while one in the OC group developed postoperative 1. Taki-Eldin A, Badawy AE. Outcome of laparoscopic cholecystectomy
adhesion. There was no conversion from LC to OC, no difference in in patients with gallstone disease at a secondary level care
postoperative analgesia, no surgical site infection noted, and no hospital. Arq Bras Cir Dig 2018;31(1):e1347. DOI: 10.1590/0102-
mortality recorded. 672020180001e1347.
2. Polychronidis A, Laftsidis P, et al. Twenty years of laparoscopic
dIscussIon cholecystectomy: Philippe Mouret—March 17, 1987. JSLS
2008;12(1):109–111.
The low volume of patients can be explained by the rarity of 3. Lombardo S, Rosenberg JS, et al. Cost and outcomes of open vs
11
these cases in our environment. Although the trend is changing, laparoscopic cholecystectomy in Mongolia. J Surg Res 2018;229:
12,13
especially with the introduction of LC. 186–191. DOI: 10.1016/j.jss.2018.03.036.
The female-to-male ratio was 1.2:1 as against 5:1 seen in 4. Hussain A, Mahmood HK, et al. Laparoscopic cholecystectomy
11,12
other studies. This was surprising since gallstones were more can be safely performed in a resource-limited setting: the first 49
common in females than in males. It could be that less females laparoscopic cholecystectomies in Yemen. JSLS 2008;12(1):71–76.
presented due to may be religious and/or cultural reasons. The 5. Sanogo ZZ, Sangare D, et al. Laparoscopic cholecystectomy. The first
30 cases in Bamako. Mali Med 2006;21(2):15–22.
11
mean age was 39 years as seen also in a study by Asuquo et al. 6. Ekwunife CN, Njike CI. Intent at day case laparoscopic cholecystectomy
Symptomatic gallstones were the indication in all patients except in owerri, Nigeria: initial experiences. Nig J Surg 2013;19(1):16–18. DOI:
in one which was for an acalculous cholecystitis. The same was 10.4103/1117-6806.111501.
World Journal of Laparoscopic Surgery, Volume 11 Issue 3 (September–December 2018) 133