Page 48 - Journal of World Association of Laparoscopic Surgeons
P. 48
Laparoscopic Management of Median Arcuate Ligament Syndrome: Single Center Experience
Fig. 2: A CT angiography image of the patient (sagittal view) showing Fig. 3: A CT angiography image (axial view) showing compression of
compression of the celiac trunk with post stenotic dilatation the celiac trunk with post stenotic dilatation
up to 2 years, the patient is significantly pain free, tolerating the
diet well.
Case 2
A 22-year-old lady came with chief complaints of severe epigastric
abdominal pain aggravated for 5 days, with a history of similar
complaints for the last 2 years, and moderate severity aggravated
by food intake. A history of nausea was present on and off. No
history of vomiting or fever was found to be associated with the
symptoms. A history of approx 10 kg loss of weight was present in
the last 6 months.
Upper GI endoscopy and colonoscopy normal. CECT abdomen
revealed significant compression on the proximal part of the celiac
artery by median arcuate ligament—suggestive of MALS.
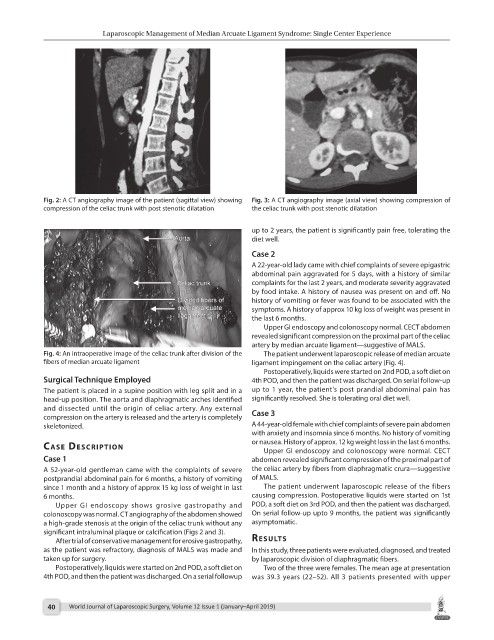
Fig. 4: An intraoperative image of the celiac trunk after division of the The patient underwent laparoscopic release of median arcuate
fibers of median arcuate ligament ligament impingement on the celiac artery (Fig. 4).
Postoperatively, liquids were started on 2nd POD, a soft diet on
Surgical Technique Employed 4th POD, and then the patient was discharged. On serial follow-up
The patient is placed in a supine position with leg split and in a up to 1 year, the patient’s post prandial abdominal pain has
head-up position. The aorta and diaphragmatic arches identified significantly resolved. She is tolerating oral diet well.
and dissected until the origin of celiac artery. Any external
compression on the artery is released and the artery is completely Case 3
skeletonized. A 44-year-old female with chief complaints of severe pain abdomen
with anxiety and insomnia since 6 months. No history of vomiting
or nausea. History of approx. 12 kg weight loss in the last 6 months.
cAse descrIptIon Upper GI endoscopy and colonoscopy were normal. CECT
Case 1 abdomen revealed significant compression of the proximal part of
A 52-year-old gentleman came with the complaints of severe the celiac artery by fibers from diaphragmatic crura—suggestive
postprandial abdominal pain for 6 months, a history of vomiting of MALS.
since 1 month and a history of approx 15 kg loss of weight in last The patient underwent laparoscopic release of the fibers
6 months. causing compression. Postoperative liquids were started on 1st
Upper GI endoscopy shows grosive gastropathy and POD, a soft diet on 3rd POD, and then the patient was discharged.
colonoscopy was normal. CT angiography of the abdomen showed On serial follow-up upto 9 months, the patient was significantly
a high-grade stenosis at the origin of the celiac trunk without any asymptomatic.
significant intraluminal plaque or calcification (Figs 2 and 3).
After trial of conservative management for erosive gastropathy, results
as the patient was refractory, diagnosis of MALS was made and In this study, three patients were evaluated, diagnosed, and treated
taken up for surgery. by laparoscopic division of diaphragmatic fibers.
Postoperatively, liquids were started on 2nd POD, a soft diet on Two of the three were females. The mean age at presentation
4th POD, and then the patient was discharged. On a serial followup was 39.3 years (22–52). All 3 patients presented with upper
40 World Journal of Laparoscopic Surgery, Volume 12 Issue 1 (January–April 2019)