Page 43 - Journal of World Association of Laparoscopic Surgeons
P. 43
Pain Relief After LVHR
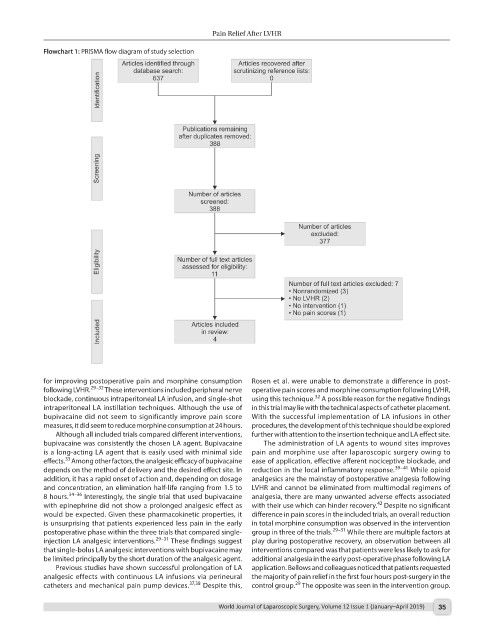
Flowchart 1: PRISMA flow diagram of study selection
for improving postoperative pain and morphine consumption Rosen et al. were unable to demonstrate a difference in post-
29–32
following LVHR. These interventions included peripheral nerve operative pain scores and morphine consumption following LVHR,
32
blockade, continuous intraperitoneal LA infusion, and single-shot using this technique. A possible reason for the negative findings
intraperitoneal LA instillation techniques. Although the use of in this trial may lie with the technical aspects of catheter placement.
bupivacaine did not seem to significantly improve pain score With the successful implementation of LA infusions in other
measures, it did seem to reduce morphine consumption at 24 hours. procedures, the development of this technique should be explored
Although all included trials compared different interventions, further with attention to the insertion technique and LA effect site.
bupivacaine was consistently the chosen LA agent. Bupivacaine The administration of LA agents to wound sites improves
is a long-acting LA agent that is easily used with minimal side pain and morphine use after laparoscopic surgery owing to
33
effects. Among other factors, the analgesic efficacy of bupivacaine ease of application, effective afferent nociceptive blockade, and
39–41
depends on the method of delivery and the desired effect site. In reduction in the local inflammatory response. While opioid
addition, it has a rapid onset of action and, depending on dosage analgesics are the mainstay of postoperative analgesia following
and concentration, an elimination half-life ranging from 1.5 to LVHR and cannot be eliminated from multimodal regimens of
34–36
8 hours. Interestingly, the single trial that used bupivacaine analgesia, there are many unwanted adverse effects associated
42
with epinephrine did not show a prolonged analgesic effect as with their use which can hinder recovery. Despite no significant
would be expected. Given these pharmacokinetic properties, it difference in pain scores in the included trials, an overall reduction
is unsurprising that patients experienced less pain in the early in total morphine consumption was observed in the intervention
29–31
postoperative phase within the three trials that compared single- group in three of the trials. While there are multiple factors at
29–31
injection LA analgesic interventions. These findings suggest play during postoperative recovery, an observation between all
that single-bolus LA analgesic interventions with bupivacaine may interventions compared was that patients were less likely to ask for
be limited principally by the short duration of the analgesic agent. additional analgesia in the early post-operative phase following LA
Previous studies have shown successful prolongation of LA application. Bellows and colleagues noticed that patients requested
analgesic effects with continuous LA infusions via perineural the majority of pain relief in the first four hours post-surgery in the
37,38
29
catheters and mechanical pain pump devices. Despite this, control group. The opposite was seen in the intervention group.
World Journal of Laparoscopic Surgery, Volume 12 Issue 1 (January–April 2019) 35