Page 38 - Journal of World Association of Laparoscopic Surgeons
P. 38
Comparison between RYGB and MGB in Patients of Developing Countries
A specified number of bariatric surgeries of RYGB and MGB done result
were analyzed over several variables.
The result was on the parameters of operation time, operative
morbidities follow-up, and Quality of Life Assessment survey. A
mAterIAls And methods multicenter study of 500 MGBs and 500 RYGB done in 5 years in
This a multicenter survey in which there is a detailed review the developing country revealed the mortality rate to be 0.3%
of cases done in specialized hospitals in developing countries in RYGB and zero in MGB. A comparative analysis of results is as
assisted by search engines such as MSN, etc., using Springer Link indicated in Table 1.
and the Journal of Minimal Access Surgery (MAS). Bariatric-specific Bile reflux was <1% in the MGB series and nil in RYGB.
longitudinal data analyzed for complication and benefits formed In both, there was no persistent vomiting, and the weight regain
the bedrock of assessment in the comparison of MGB and RYGB. was 8.5% in RYGB but 0% in MGB.
Hypoalbuminemia was 2% in RYGB and 13.17 in MGB.
Operative Techniques Hypertension, type 2 diabetes, dyslipidemia, and percent excess
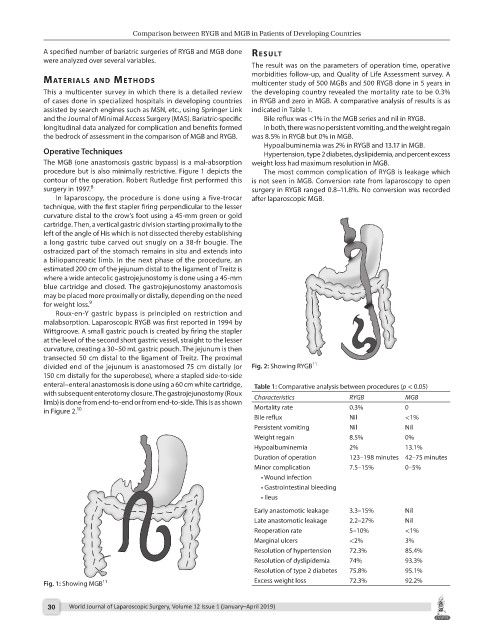
The MGB (one anastomosis gastric bypass) is a mal-absorption weight loss had maximum resolution in MGB.
procedure but is also minimally restrictive. Figure 1 depicts the The most common complication of RYGB is leakage which
contour of the operation. Robert Rutledge first performed this is not seen in MGB. Conversion rate from laparoscopy to open
8
surgery in 1997. surgery in RYGB ranged 0.8–11.8%. No conversion was recorded
In laparoscopy, the procedure is done using a five-trocar after laparoscopic MGB.
technique, with the first stapler firing perpendicular to the lesser
curvature distal to the crow’s foot using a 45-mm green or gold
cartridge. Then, a vertical gastric division starting proximally to the
left of the angle of His which is not dissected thereby establishing
a long gastric tube carved out snugly on a 38-fr bougie. The
ostracized part of the stomach remains in situ and extends into
a biliopancreatic limb. In the next phase of the procedure, an
estimated 200 cm of the jejunum distal to the ligament of Treitz is
where a wide antecolic gastrojejunostomy is done using a 45-mm
blue cartridge and closed. The gastrojejunostomy anastomosis
may be placed more proximally or distally, depending on the need
9
for weight loss.
Roux-en-Y gastric bypass is principled on restriction and
malabsorption. Laparoscopic RYGB was first reported in 1994 by
Wittgroove. A small gastric pouch is created by firing the stapler
at the level of the second short gastric vessel, straight to the lesser
curvature, creating a 30–50 mL gastric pouch. The jejunum is then
transected 50 cm distal to the ligament of Treitz. The proximal
11
divided end of the jejunum is anastomosed 75 cm distally (or Fig. 2: Showing RYGB
150 cm distally for the superobese), where a stapled side-to-side
enteral–enteral anastomosis is done using a 60 cm white cartridge, Table 1: Comparative analysis between procedures (p < 0.05)
with subsequent enterotomy closure. The gastrojejunostomy (Roux Characteristics RYGB MGB
limb) is done from end-to-end or from end-to-side. This is as shown
in Figure 2. 10 Mortality rate 0.3% 0
Bile reflux Nil <1%
Persistent vomiting Nil Nil
Weight regain 8.5% 0%
Hypoalbuminemia 2% 13.1%
Duration of operation 123–198 minutes 42–75 minutes
Minor complication 7.5–15% 0–5%
• Wound infection
• Gastrointestinal bleeding
• Ileus
Early anastomotic leakage 3.3–15% Nil
Late anastomotic leakage 2.2–27% Nil
Reoperation rate 5–10% <1%
Marginal ulcers <2% 3%
Resolution of hypertension 72.3% 85.4%
Resolution of dyslipidemia 74% 93.3%
Resolution of type 2 diabetes 75.8% 95.1%
11
Fig. 1: Showing MGB Excess weight loss 72.3% 92.2%
30 World Journal of Laparoscopic Surgery, Volume 12 Issue 1 (January–April 2019)