Page 19 - Journal of World Association of Laparoscopic Surgeons
P. 19
Study of Feasibility of Single Incision Laparoscopic Surgery with Conventional Instruments
2 belong to cholecystectomy group. Postoperative pain was more than 5. Mean analgesic dose requirement was 2.52 ± 0.60
measured by using VAS, ranging from 0–10, every 6 hours for doses in appendectomy group while it was 2.94 ± 0.62 doses in
first 24 hours and average of the 4 scores was taken. Mean VAS cholecystectomy group.
score in first 24 hours was 5.38 ± 0.58 in appendectomy group Port-site infection occurred in two cases, one from
while it was 6 ± 0.74 in cholecystectomy group. VAS score was appendectomy and one from cholecystectomy group. In both
obtained at a point of time, postoperative day 2 in every patient, cases, it was cellulitis around infraumbilical port and was managed
and mean VAS score on POD 2 was 2.14 ± in appendectomy conservatively in both cases. Patients were encouraged for
group while it was 2.21 ± 0.53 in cholecystectomy group. Patient mobilization postoperatively as soon as they were comfortable.
received 50 mg of Inj. Diclofenac sodium in first 24 hours as per Patients were discharged from hospital once adequately mobilized
VAS score. One dose was given every time when VAS score was and have good pain relief. Mean postoperative hospital stay in
appendectomy group was 2.09 ± 0.30 days while it was 2.10 ± 0.31
days in cholecystectomy group. Mean time to return to normal
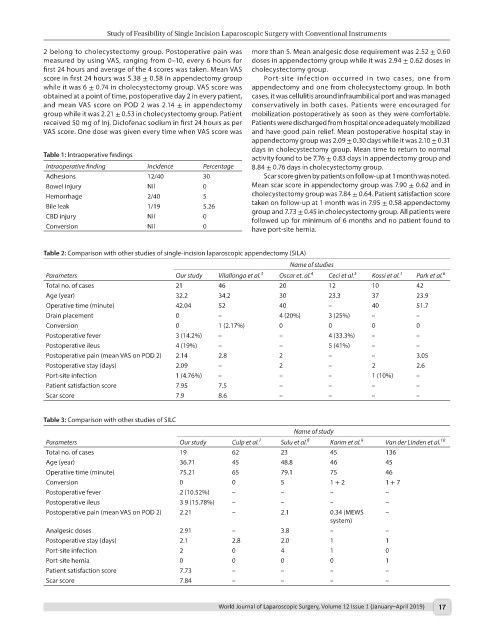
Table 1: Intraoperative findings
activity found to be 7.76 ± 0.83 days in appendectomy group and
Intraoperative finding Incidence Percentage 8.84 ± 0.76 days in cholecystectomy group.
Adhesions 12/40 30 Scar score given by patients on follow-up at 1 month was noted.
Bowel injury Nil 0 Mean scar score in appendectomy group was 7.90 ± 0.62 and in
Hemorrhage 2/40 5 cholecystectomy group was 7.84 ± 0.64. Patient satisfaction score
Bile leak 1/19 5.26 taken on follow-up at 1 month was in 7.95 ± 0.58 appendectomy
group and 7.73 ± 0.45 in cholecystectomy group. All patients were
CBD injury Nil 0 followed up for minimum of 6 months and no patient found to
Conversion Nil 0 have port-site hernia.
Table 2: Comparison with other studies of single-incision laparoscopic appendectomy (SILA)
Name of studies
Parameters Our study Vilallonga et al. 3 Oscar et. al. 4 Ceci et al. 5 Kossi et al. 1 Park et al. 6
Total no. of cases 21 46 20 12 10 42
Age (year) 32.2 34.2 30 23.3 37 23.9
Operative time (minute) 42.04 52 40 – 40 51.7
Drain placement 0 – 4 (20%) 3 (25%) – –
Conversion 0 1 (2.17%) 0 0 0 0
Postoperative fever 3 (14.2%) – – 4 (33.3%) – –
Postoperative ileus 4 (19%) – – 5 (41%) – –
Postoperative pain (mean VAS on POD 2) 2.14 2.8 2 – – 3.05
Postoperative stay (days) 2.09 – 2 – 2 2.6
Port-site infection 1 (4.76%) – – – 1 (10%) –
Patient satisfaction score 7.95 7.5 – – – –
Scar score 7.9 8.6 – – – –
Table 3: Comparison with other studies of SILC
Name of study
Parameters Our study Culp et al. 7 Sulu et al. 8 Karim et al. 9 Van der Linden et al. 10
Total no. of cases 19 62 23 45 136
Age (year) 36.71 45 48.8 46 45
Operative time (minute) 75.21 65 79.1 75 46
Conversion 0 0 5 1 + 2 1 + 7
Postoperative fever 2 (10.52%) – – – –
Postoperative ileus 3 9 (15.78%) – – – –
Postoperative pain (mean VAS on POD 2) 2.21 – 2.1 0.34 (MEWS –
system)
Analgesic doses 2.91 – 3.8 – –
Postoperative stay (days) 2.1 2.8 2.0 1 1
Port-site infection 2 0 4 1 0
Port-site hernia 0 0 0 0 1
Patient satisfaction score 7.73 – – – –
Scar score 7.84 – – – –
World Journal of Laparoscopic Surgery, Volume 12 Issue 1 (January–April 2019) 17