Page 23 - Journal of World Association of Laparoscopic Surgeons
P. 23
Comparative Analysis of Surgical and Pathological Outcomes
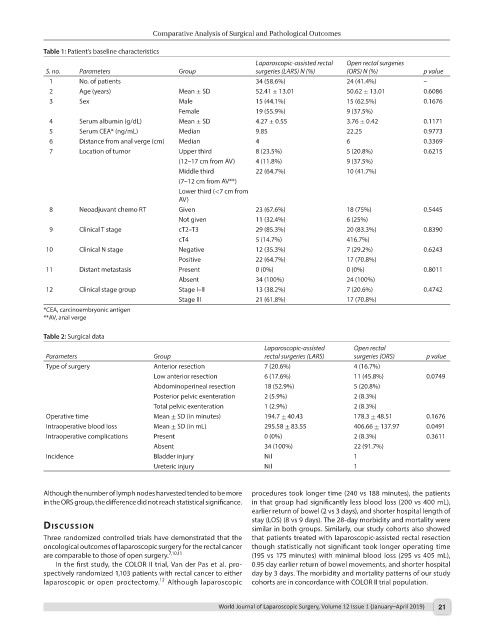
Table 1: Patient’s baseline characteristics
Laparoscopic-assisted rectal Open rectal surgeries
S. no. Parameters Group surgeries (LARS) N (%) (ORS) N (%) p value
1 No. of patients 34 (58.6%) 24 (41.4%) –
2 Age (years) Mean ± SD 52.41 ± 13.01 50.62 ± 13.01 0.6086
3 Sex Male 15 (44.1%) 15 (62.5%) 0.1676
Female 19 (55.9%) 9 (37.5%)
4 Serum albumin (g/dL) Mean ± SD 4.27 ± 0.55 3.76 ± 0.42 0.1171
5 Serum CEA* (ng/mL) Median 9.85 22.25 0.9773
6 Distance from anal verge (cm) Median 4 6 0.3369
7 Location of tumor Upper third 8 (23.5%) 5 (20.8%) 0.6215
(12–17 cm from AV) 4 (11.8%) 9 (37.5%)
Middle third 22 (64.7%) 10 (41.7%)
(7–12 cm from AV**)
Lower third (<7 cm from
AV)
8 Neoadjuvant chemo RT Given 23 (67.6%) 18 (75%) 0.5445
Not given 11 (32.4%) 6 (25%)
9 Clinical T stage cT2–T3 29 (85.3%) 20 (83.3%) 0.8390
cT4 5 (14.7%) 416.7%)
10 Clinical N stage Negative 12 (35.3%) 7 (29.2%) 0.6243
Positive 22 (64.7%) 17 (70.8%)
11 Distant metastasis Present 0 (0%) 0 (0%) 0.8011
Absent 34 (100%) 24 (100%)
12 Clinical stage group Stage I–II 13 (38.2%) 7 (20.6%) 0.4742
Stage III 21 (61.8%) 17 (70.8%)
*CEA, carcinoembryonic antigen
**AV, anal verge
Table 2: Surgical data
Laparoscopic-assisted Open rectal
Parameters Group rectal surgeries (LARS) surgeries (ORS) p value
Type of surgery Anterior resection 7 (20.6%) 4 (16.7%)
Low anterior resection 6 (17.6%) 11 (45.8%) 0.0749
Abdominoperineal resection 18 (52.9%) 5 (20.8%)
Posterior pelvic exenteration 2 (5.9%) 2 (8.3%)
Total pelvic exenteration 1 (2.9%) 2 (8.3%)
Operative time Mean ± SD (in minutes) 194.7 ± 40.43 178.3 ± 48.51 0.1676
Intraoperative blood loss Mean ± SD (in mL) 295.58 ± 83.55 406.66 ± 137.97 0.0491
Intraoperative complications Present 0 (0%) 2 (8.3%) 0.3611
Absent 34 (100%) 22 (91.7%)
Incidence Bladder injury Nil 1
Ureteric injury Nil 1
Although the number of lymph nodes harvested tended to be more procedures took longer time (240 vs 188 minutes), the patients
in the ORS group, the difference did not reach statistical significance. in that group had significantly less blood loss (200 vs 400 mL),
earlier return of bowel (2 vs 3 days), and shorter hospital length of
stay (LOS) (8 vs 9 days). The 28-day morbidity and mortality were
dIscussIon similar in both groups. Similarly, our study cohorts also showed
Three randomized controlled trials have demonstrated that the that patients treated with laparoscopic-assisted rectal resection
oncological outcomes of laparoscopic surgery for the rectal cancer though statistically not significant took longer operating time
are comparable to those of open surgery. 7,10,11 (195 vs 175 minutes) with minimal blood loss (295 vs 405 mL),
In the first study, the COLOR II trial, Van der Pas et al. pro- 0.95 day earlier return of bowel movements, and shorter hospital
spectively randomized 1,103 patients with rectal cancer to either day by 3 days. The morbidity and mortality patterns of our study
12
laparoscopic or open proctectomy. Although laparoscopic cohorts are in concordance with COLOR II trial population.
World Journal of Laparoscopic Surgery, Volume 12 Issue 1 (January–April 2019) 21