Page 9 - World Journal of Laparoscopic Surgery
P. 9
Laparoscopic vs Mini-incision Open Appendectomy
stump leak. The peritoneum and fascia were approximated using while categorical variables were expressed as frequencies and
2/0 vicryl sutures. The incision in the skin was closed by using 1/0 percentages. Graphically, the data was presented by bar diagrams.
non-absorbable suture. Student’s independent t-test was used for comparing continuous
variables, while Chi-squared test or Fisher’s exact test was used
Postoperative Course for comparing categorical variables. A p <0.05 was considered
In the postoperative period intravenous fluids were continued for statistically significant. All p values were two-tailed ones.
12 hours. All patients were given two doses of third-generation
cephalosporin, one dose was given at the time of intubation
and another was given 12 hours after surgery. Patients with results And observAtIons
complicated appendicitis received a combination of third- The total number of patients studied was 101, out of which 52
generation cephalosporin and metronidazole. For purpose of were taken for MIA and 49 for LA. We did not convert any of the
analgesia, all patients were put on paracetamol infusion during the laparoscopic procedures to open surgery.
procedure followed by 75-mg intramuscular diclofenac sodium as The patients who were taken for MIA had a mean age of 31.9
and when needed. (13.06) years, while the patients who were taken for LA group had
During the postoperative period, pulse rate, blood pressure, a mean age of 32.4 (14.34) years (Table 1). Thus, both groups were
temperature, and respiratory rate were monitored in all patients. comparable as far as the age is concerned, with no statistically
All patients were monitored for VAS at 6, 12, and 24 hours after significant difference (p >0.05). In MIA group, out of 52 patients, 31
surgery and same was recorded in the already prepared pro (59.6%) were males and 21 (40.4%) were females, while in LA group,
forma. The patients were allowed to take a clear liquid diet once out of 49 patients, 24 (49%) were males and 25 (51%) were females
the bowel sounds were present, followed by a regular diet. The with p >0.05, which is statistically insignificant.
patients were monitored for various clinical parameters which were The patients who underwent MIA had an operating time
recorded in already prepared pro forma. These parameters included ranging from 30–35 minutes, with a mean of 32.7 (2.52) while
total operative time, number of doses of analgesia received in patients who were subjected to LA had the operative time ranging
the immediate postoperative period, time taken to resume oral from 25–30 minutes, with a mean of 26.9 (2.46). The difference in
intake, pain score, hospital stay, and complications if any. Pain operating time was statistically significant in favor of LA (p <0.001)
score was assessed independently by the resident doctors using (Table 1).
10-cm unscaled VAS. The patients were advised to take tablet of Intraoperative bleeding was seen in 2 (3.84%) patients
aceclofenac 100 mg as an analgesia as and when needed. Total belonging to MIA group while another 2 (3.84%) patients had an
operative time was calculated from the time of incision in the skin iatrogenic injury to bowel. No such complication was seen in any
till the placement of last suture. of the patients taken for laparoscopy (p >0.05) (Table 2).
The patients were discharged on oral antibiotics and were The patients belonging to LA group experienced less pain in
advised to take analgesic tablets as and when needed and to contrast to MIA group on a VAS. The overall pain score in MIA was
keep a record of it. The follow-up was done in the outpatient clinic 2.86 (1.184) in MIA and 2.30 (1.022) in case of LA. This difference in
at weekly intervals for a period of 1 month. During follow-up, a pain between the two groups was statistically significant with a
detailed history was taken and thorough examination was done p <0.001 (Table 1).
as per the pro forma. The number of injectable analgesics needed during the first
24 hours after surgery was significantly higher in MIA group
Statistical Analysis as compared to LA group with p = 0.002, which is statistically
All observed data was compiled and entered in a spreadsheet significant (p <0.05). After discharge from the hospital, the number
(Microsoft Excel) and then exported to data editor of Statistical of analgesic tablets taken by patients who underwent LA was less
Package for Social Sciences (SPSS), version 20.0 (SPSS Inc. Chicago, as compared to patients who underwent MIA, which was again
Illinois, USA). Continuous variables were expressed as mean (SD), statistically significant (Table 1).
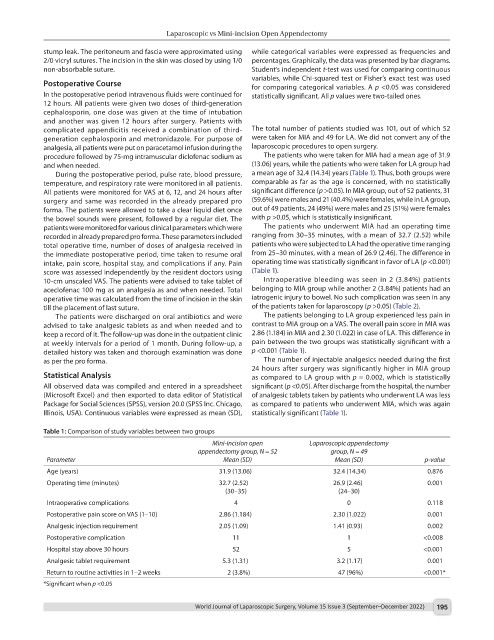
Table 1: Comparison of study variables between two groups
Mini-incision open Laparoscopic appendectomy
appendectomy group, N = 52 group, N = 49
Parameter Mean (SD) Mean (SD) p-value
Age (years) 31.9 (13.06) 32.4 (14.34) 0.876
Operating time (minutes) 32.7 (2.52) 26.9 (2.46) 0.001
(30–35) (24–30)
Intraoperative complications 4 0 0.118
Postoperative pain score on VAS (1–10) 2.86 (1.184) 2.30 (1.022) 0.001
Analgesic injection requirement 2.05 (1.09) 1.41 (0.93) 0.002
Postoperative complication 11 1 <0.008
Hospital stay above 30 hours 52 5 <0.001
Analgesic tablet requirement 5.3 (1.31) 3.2 (1.17) 0.001
Return to routine activities in 1–2 weeks 2 (3.8%) 47 (96%) <0.001*
*Significant when p <0.05
World Journal of Laparoscopic Surgery, Volume 15 Issue 3 (September–December 2022) 195