Page 8 - World Journal of Laparoscopic Surgery
P. 8
Laparoscopic vs Mini-incision Open Appendectomy
analgesic requirement, postoperative complications, number of
days in the hospital, time taken to return routine work and cosmetic
results.
mAterIAls And methods
This study was a prospective study conducted from July 2017 to
June 2019 in the Department of General and Minimal Invasive
Surgery, SKIMS Medical College, Bemina, Srinagar.
The study included all adult patients admitted in the department
of surgery with a diagnosis of acute appendicitis. The patients were
randomly taken either for LA or MIA. The total number of patients
studied was 101. Laparoscopic appendectomy was done in 49
patients while MIA was done in 52 patients. The patients excluded
from the study included those who were symptomatic for more than
5 days, those with a palpable right lower abdominal mass, those
with features of peritonitis and shock at the time of presentation,
patients with large abdominal hernia, patients with previous history
of laparotomies, patients with a severe cardiopulmonary disease,
patients with coagulation disorders and cirrhotic liver and all
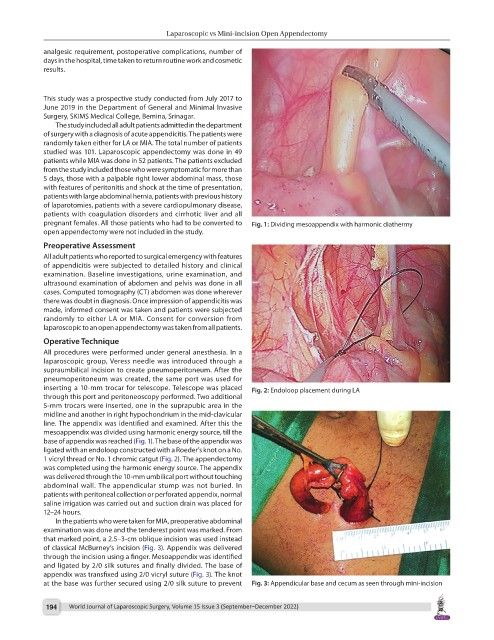
pregnant females. All those patients who had to be converted to Fig. 1: Dividing mesoappendix with harmonic diathermy
open appendectomy were not included in the study.
Preoperative Assessment
All adult patients who reported to surgical emergency with features
of appendicitis were subjected to detailed history and clinical
examination. Baseline investigations, urine examination, and
ultrasound examination of abdomen and pelvis was done in all
cases. Computed tomography (CT) abdomen was done wherever
there was doubt in diagnosis. Once impression of appendicitis was
made, informed consent was taken and patients were subjected
randomly to either LA or MIA. Consent for conversion from
laparoscopic to an open appendectomy was taken from all patients.
Operative Technique
All procedures were performed under general anesthesia. In a
laparoscopic group, Veress needle was introduced through a
supraumbilical incision to create pneumoperitoneum. After the
pneumoperitoneum was created, the same port was used for
inserting a 10-mm trocar for telescope. Telescope was placed Fig. 2: Endoloop placement during LA
through this port and peritoneoscopy performed. Two additional
5-mm trocars were inserted, one in the suprapubic area in the
midline and another in right hypochondrium in the mid-clavicular
line. The appendix was identified and examined. After this the
mesoappendix was divided using harmonic energy source, till the
base of appendix was reached (Fig. 1). The base of the appendix was
ligated with an endoloop constructed with a Roeder’s knot on a No.
1 vicryl thread or No. 1 chromic catgut (Fig. 2). The appendectomy
was completed using the harmonic energy source. The appendix
was delivered through the 10-mm umbilical port without touching
abdominal wall. The appendicular stump was not buried. In
patients with peritoneal collection or perforated appendix, normal
saline irrigation was carried out and suction drain was placed for
12–24 hours.
In the patients who were taken for MIA, preoperative abdominal
examination was done and the tenderest point was marked. From
that marked point, a 2.5–3-cm oblique incision was used instead
of classical McBurney’s incision (Fig. 3). Appendix was delivered
through the incision using a finger. Mesoappendix was identified
and ligated by 2/0 silk sutures and finally divided. The base of
appendix was transfixed using 2/0 vicryl suture (Fig. 3). The knot
at the base was further secured using 2/0 silk suture to prevent Fig. 3: Appendicular base and cecum as seen through mini-incision
194 World Journal of Laparoscopic Surgery, Volume 15 Issue 3 (September–December 2022)