Page 84 - World Journal of Laparoscopic Surgery
P. 84
LSG in Obesity and GERD
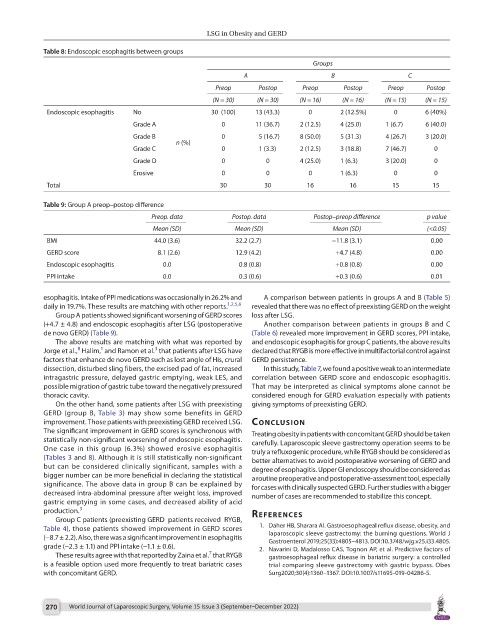
Table 8: Endoscopic esophagitis between groups
Groups
A B C
Preop Postop Preop Postop Preop Postop
(N = 30) (N = 30) (N = 16) (N = 16) (N = 15) (N = 15)
Endoscopic esophagitis No 30 (100) 13 (43.3) 0 2 (12.5%) 0 6 (40%)
Grade A 0 11 (36.7) 2 (12.5) 4 (25.0) 1 (6.7) 6 (40.0)
Grade B 0 5 (16.7) 8 (50.0) 5 (31.3) 4 (26.7) 3 (20.0)
n (%)
Grade C 0 1 (3.3) 2 (12.5) 3 (18.8) 7 (46.7) 0
Grade D 0 0 4 (25.0) 1 (6.3) 3 (20.0) 0
Erosive 0 0 0 1 (6.3) 0 0
Total 30 30 16 16 15 15
Table 9: Group A preop–postop difference
Preop. data Postop. data Postop–preop difference p value
Mean (SD) Mean (SD) Mean (SD) (<0.05)
BMI 44.0 (3.6) 32.2 (2.7) −11.8 (3.1) 0.00
GERD score 8.1 (2.6) 12.9 (4.2) +4.7 (4.8) 0.00
Endoscopic esophagitis 0.0 0.8 (0.8) +0.8 (0.8) 0.00
PPI intake 0.0 0.3 (0.6) +0.3 (0.6) 0.01
esophagitis. Intake of PPI medications was occasionally in 26.2% and A comparison between patients in groups A and B (Table 5)
daily in 19.7%. These results are matching with other reports. 1,2,5,6 revealed that there was no effect of preexisting GERD on the weight
Group A patients showed significant worsening of GERD scores loss after LSG.
(+4.7 ± 4.8) and endoscopic esophagitis after LSG (postoperative Another comparison between patients in groups B and C
de novo GERD) (Table 9). (Table 6) revealed more improvement in GERD scores, PPI intake,
The above results are matching with what was reported by and endoscopic esophagitis for group C patients, the above results
3
8
1
Jorge et al., Halim, and Ramon et al. that patients after LSG have declared that RYGB is more effective in multifactorial control against
factors that enhance de novo GERD such as lost angle of His, crural GERD persistence.
dissection, disturbed sling fibers, the excised pad of fat, increased In this study, Table 7, we found a positive weak to an intermediate
intragastric pressure, delayed gastric emptying, weak LES, and correlation between GERD score and endoscopic esophagitis.
possible migration of gastric tube toward the negatively pressured That may be interpreted as clinical symptoms alone cannot be
thoracic cavity. considered enough for GERD evaluation especially with patients
On the other hand, some patients after LSG with preexisting giving symptoms of preexisting GERD.
GERD (group B, Table 3) may show some benefits in GERD
improvement. Those patients with preexisting GERD received LSG. conclusIon
The significant improvement in GERD scores is synchronous with Treating obesity in patients with concomitant GERD should be taken
statistically non-significant worsening of endoscopic esophagitis. carefully. Laparoscopic sleeve gastrectomy operation seems to be
One case in this group (6.3%) showed erosive esophagitis truly a refluxogenic procedure, while RYGB should be considered as
(Tables 3 and 8). Although it is still statistically non-significant better alternatives to avoid postoperative worsening of GERD and
but can be considered clinically significant, samples with a degree of esophagitis. Upper GI endoscopy should be considered as
bigger number can be more beneficial in declaring the statistical a routine preoperative and postoperative-assessment tool, especially
significance. The above data in group B can be explained by for cases with clinically suspected GERD. Further studies with a bigger
decreased intra-abdominal pressure after weight loss, improved number of cases are recommended to stabilize this concept.
gastric emptying in some cases, and decreased ability of acid
production. 3 references
Group C patients (preexisting GERD patients received RYGB,
Table 4), those patients showed improvement in GERD scores 1. Daher HB, Sharara AI. Gastroesophageal reflux disease, obesity, and
(−8.7 ± 2.2). Also, there was a significant improvement in esophagitis laparoscopic sleeve gastrectomy: the burning questions. World J
Gastroenterol 2019;25(33):4805–4813. DOI:10.3748/wjg.v25.i33.4805.
grade (−2.3 ± 1.1) and PPI intake (−1.1 ± 0.6). 2. Navarini D, Madalosso CAS, Tognon AP, et al. Predictive factors of
7
These results agree with that reported by Zaina et al. that RYGB gastroesophageal reflux disease in bariatric surgery: a controlled
is a feasible option used more frequently to treat bariatric cases trial comparing sleeve gastrectomy with gastric bypass. Obes
with concomitant GERD. Surg2020;30(4):1360–1367. DOI:10.1007/s11695-019-04286-5.
270 World Journal of Laparoscopic Surgery, Volume 15 Issue 3 (September–December 2022)