Page 87 - World Journal of Laparoscopic Surgery
P. 87
A Safe Scarless Appendectomy
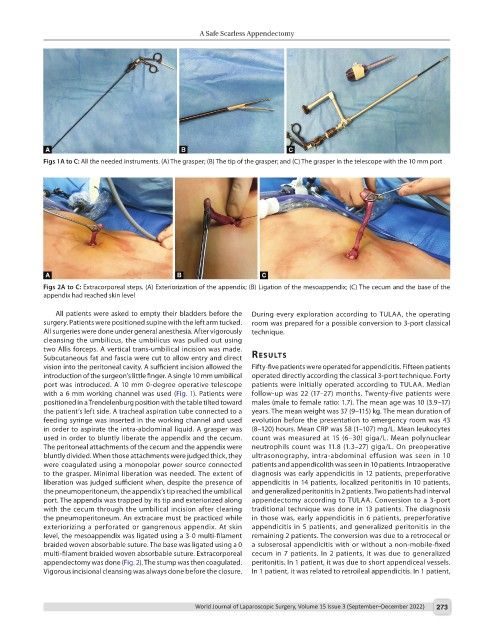
Figs 1A to C: All the needed instruments. (A) The grasper; (B) The tip of the grasper; and (C) The grasper in the telescope with the 10 mm port
Figs 2A to C: Extracorporeal steps. (A) Exteriorization of the appendix; (B) Ligation of the mesoappendix; (C) The cecum and the base of the
appendix had reached skin level
All patients were asked to empty their bladders before the During every exploration according to TULAA, the operating
surgery. Patients were positioned supine with the left arm tucked. room was prepared for a possible conversion to 3-port classical
All surgeries were done under general anesthesia. After vigorously technique.
cleansing the umbilicus, the umbilicus was pulled out using
two Allis forceps. A vertical trans-umbilical incision was made.
Subcutaneous fat and fascia were cut to allow entry and direct results
vision into the peritoneal cavity. A sufficient incision allowed the Fifty-five patients were operated for appendicitis. Fifteen patients
introduction of the surgeon’s little finger. A single 10 mm umbilical operated directly according the classical 3-port technique. Forty
port was introduced. A 10 mm 0-degree operative telescope patients were initially operated according to TULAA. Median
with a 6 mm working channel was used (Fig. 1). Patients were follow-up was 22 (17–27) months. Twenty-five patients were
positioned in a Trendelenburg position with the table tilted toward males (male to female ratio: 1.7). The mean age was 10 (3.9–17)
the patient’s left side. A tracheal aspiration tube connected to a years. The mean weight was 37 (9–115) kg. The mean duration of
feeding syringe was inserted in the working channel and used evolution before the presentation to emergency room was 43
in order to aspirate the intra-abdominal liquid. A grasper was (8–120) hours. Mean CRP was 58 (1–107) mg/L. Mean leukocytes
used in order to bluntly liberate the appendix and the cecum. count was measured at 15 (6–30) giga/L. Mean polynuclear
The peritoneal attachments of the cecum and the appendix were neutrophils count was 11.8 (1.3–27) giga/L. On preoperative
bluntly divided. When those attachments were judged thick, they ultrasonography, intra-abdominal effusion was seen in 10
were coagulated using a monopolar power source connected patients and appendicolith was seen in 10 patients. Intraoperative
to the grasper. Minimal liberation was needed. The extent of diagnosis was early appendicitis in 12 patients, preperforative
liberation was judged sufficient when, despite the presence of appendicitis in 14 patients, localized peritonitis in 10 patients,
the pneumoperitoneum, the appendix’s tip reached the umbilical and generalized peritonitis in 2 patients. Two patients had interval
port. The appendix was trapped by its tip and exteriorized along appendectomy according to TULAA. Conversion to a 3-port
with the cecum through the umbilical incision after clearing traditional technique was done in 13 patients. The diagnosis
the pneumoperitoneum. An extracare must be practiced while in those was, early appendicitis in 6 patients, preperforative
exteriorizing a perforated or gangrenous appendix. At skin appendicitis in 5 patients, and generalized peritonitis in the
level, the mesoappendix was ligated using a 3-0 multi-filament remaining 2 patients. The conversion was due to a retrocecal or
braided woven absorbable suture. The base was ligated using a 0 a subserosal appendicitis with or without a non-mobile-fixed
multi-filament braided woven absorbable suture. Extracorporeal cecum in 7 patients. In 2 patients, it was due to generalized
appendectomy was done (Fig. 2). The stump was then coagulated. peritonitis. In 1 patient, it was due to short appendiceal vessels.
Vigorous incisional cleansing was always done before the closure. In 1 patient, it was related to retroileal appendicitis. In 1 patient,
World Journal of Laparoscopic Surgery, Volume 15 Issue 3 (September–December 2022) 273