Page 54 - World Journal of Laparoscopic Surgery
P. 54
Laparoscopic Ventral vs Posterior Mesh Rectopexy for Rectal Prolapse
Inclusion Criteria mesorectum mobilization. A strip of polypropylene (3 × 20-cm)
All patients with rectal prolapse, either external or internal mesh was inserted and sutured as distally as possible on the anterior
prolapse. rectal wall/perineal body with three, interrupted non-absorbable
sutures (Fig. 3).
Exclusion Criteria The posterior wall of the vagina was fixed to the mesh by
Patients with comorbidities and patients with previous complicated nonabsorbable sutures. Then, the mesh was secured tension-free to
abdominal surgery. the sacral promontory via three nonabsorbable sutures. The mesh
was peritonealized by suturing the free edges of the previously
Preoperative Preparation divided peritoneum over the mesh to afford additional ventral
All patients listed for operation underwent bowel preparation for elevation of the enterocele and evade small bowel adhesions to
3 days before surgery in the form of low-fiber diet, followed by clear the mesh. 1
fluid intake and 2–3 enemata at the day before surgery.
LPMR
• Low-molecular-weight heparin (LMWH) 12 hours before surgery Laparoscopic posterior mesh rectopexy was done through
for prophylaxis against deep venous thrombosis (DVT). This was mobilization of the mesorectum posteriorly from the sacral
in addition to the elastic compression stockings worn by patients promontory to the pelvic floor. Lateral stalks were not divided.
before induction of anesthesia, Bowel resection and circumferential division of the peritoneum
• Written consents were taken from patients explaining the were not performed in this study. A T-shaped polypropylene mesh
details of surgery, the merits of minimally invasive surgery, was located with the vertical “leg” laying flush with the anterior
and illustrating the possible complications of surgery and the surface of the sacrum and held to the promontory of sacrum with
probability of change to open surgery.
three nonabsorbable sutures. The mesh “wings” were closed to
Type of Anesthesia the lateral sides of the rectum with two absorbable sutures on
2
• General anesthesia each side.
Surgical Techniques
LVMR
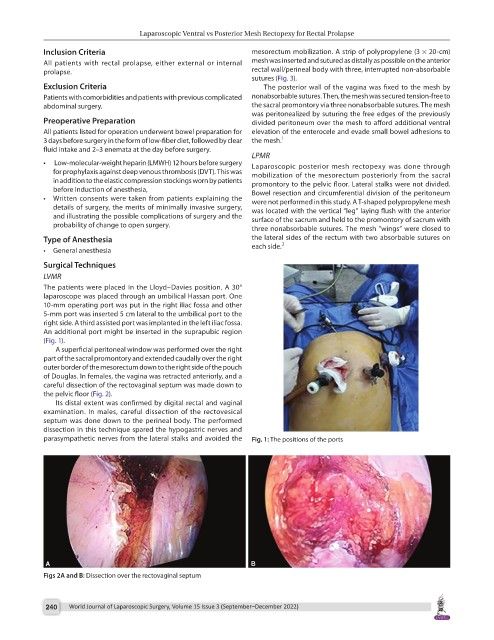
The patients were placed in the Lloyd–Davies position. A 30°
laparoscope was placed through an umbilical Hassan port. One
10-mm operating port was put in the right iliac fossa and other
5-mm port was inserted 5 cm lateral to the umbilical port to the
right side. A third assisted port was implanted in the left iliac fossa.
An additional port might be inserted in the suprapubic region
(Fig. 1).
A superficial peritoneal window was performed over the right
part of the sacral promontory and extended caudally over the right
outer border of the mesorectum down to the right side of the pouch
of Douglas. In females, the vagina was retracted anteriorly, and a
careful dissection of the rectovaginal septum was made down to
the pelvic floor (Fig. 2).
Its distal extent was confirmed by digital rectal and vaginal
examination. In males, careful dissection of the rectovesical
septum was done down to the perineal body. The performed
dissection in this technique spared the hypogastric nerves and
parasympathetic nerves from the lateral stalks and avoided the Fig. 1: The positions of the ports
Figs 2A and B: Dissection over the rectovaginal septum
240 World Journal of Laparoscopic Surgery, Volume 15 Issue 3 (September–December 2022)