Page 57 - World Journal of Laparoscopic Surgery
P. 57
Laparoscopic Ventral vs Posterior Mesh Rectopexy for Rectal Prolapse
months. As shown in Table 7, improvement of constipation was 66.09 ± 9.59 to 114.23 ± 8.64 after LVMR. The improvement is more
higher in group B in comparison with group A. in LVMR group and the difference is clinically significant.
Furthermore, one patient of group B did not improve from
incontinence. Also, two patients in group B complained persistence dIscussIon
of obstructed defecation even with correct dieting and training
for proper defecation habits. Those two patients had no prolapse Laparoscopic rectopexy has been verified to be as effective as
recurrence as shown by defecography done 3 months after open rectopexy in complete rectal prolapse treatment with
presenting of symptoms. However, one patient in group A suffered a low recurrence rate. Significant reductions in postoperative
from obstructed defecation syndrome that appeared 4 months after pain, hospital length of stay, recovery time, and complications
the operation. He had a prolapse recurrence on MRI defecography. compared with open abdominal rectopexy were encountered. The
The clinical changes after surgery were evaluated by WCS, present study compared two laparoscopic rectopexy procedures:
BPS, ODSS, as well as GIQOL. One-way ANOVA test was used for LPMR and LVMR. The comparison involved operative parameters,
comparing the changes in the functional results within each group complications, hospital length of stay, postoperative improvement
(Table 8). in fecal incontinence and constipation, as well as recurrence.
Regarding WCS, it was postoperatively lower in LVMR than LPMR Between November 2016 and 31 December 2020, forty-four patients
(6.71 ± 3.29 vs 10.78 ± 2.80, respectively). These results indicate were eligible for this study with 22 patients undergoing LPMR and
the significant improvement of constipation in group B compared 22 patients undergoing LVMR.
with group A. The postoperative decrease in BPS values proves In the present work, the mean patients’ age was 42.43 ±
the improvement of incontinence in both groups. The change was 14.05 years. There were 14 males (6 in the LPMR group vs 8 in the
statistically significant (p-value = 0.003 and 0.004 for groups A and B, LVMR group) and 30 females (16 for LPMR vs 14 for LVMR) with no
respectively). After applying ODSS, there was no difference between significant difference in-between. In this study, the rectal prolapse
the results of both groups. They showed an improvement of the incidence was higher in females. Our findings agree with those
7,8
symptoms of obstructed defecation syndrome (p-value = 0.0001). reported by Mik et al. and Madbouly and Youssef.
In group A, GIQOL score was increased from 61.00 ± 8.01 It is well-known that rectal prolapse can occur as a result of
to 105.45 ± 7.54 after surgery. While the score increased from many factors such as, chronic constipation or diarrhea long-term
history of straining during bowel movements, the weakness of
muscles, especially anal sphincter and ligaments in the rectum
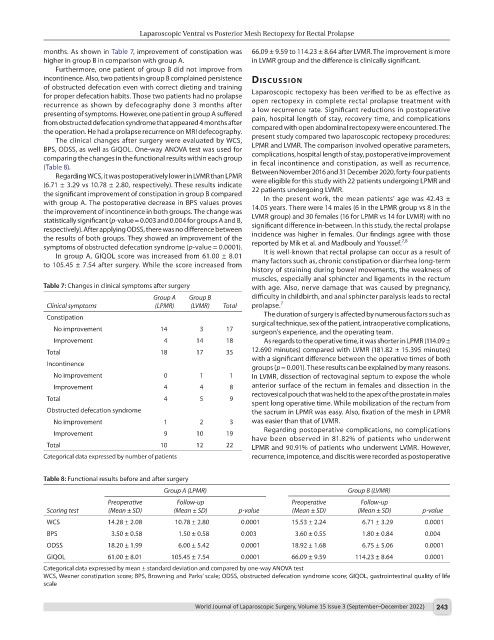
Table 7: Changes in clinical symptoms after surgery with age. Also, nerve damage that was caused by pregnancy,
Group A Group B difficulty in childbirth, and anal sphincter paralysis leads to rectal
Clinical symptoms (LPMR) (LVMR) Total prolapse. 7
Constipation The duration of surgery is affected by numerous factors such as
surgical technique, sex of the patient, intraoperative complications,
No improvement 14 3 17 surgeon’s experience, and the operating team.
Improvement 4 14 18 As regards to the operative time, it was shorter in LPMR (114.09 ±
Total 18 17 35 12.690 minutes) compared with LVMR (181.82 ± 15.395 minutes)
with a significant difference between the operative times of both
Incontinence
groups (p = 0.001). These results can be explained by many reasons.
No improvement 0 1 1 In LVMR, dissection of rectovaginal septum to expose the whole
Improvement 4 4 8 anterior surface of the rectum in females and dissection in the
rectovesical pouch that was held to the apex of the prostate in males
Total 4 5 9
spent long operative time. While mobilization of the rectum from
Obstructed defecation syndrome the sacrum in LPMR was easy. Also, fixation of the mesh in LPMR
No improvement 1 2 3 was easier than that of LVMR.
Regarding postoperative complications, no complications
Improvement 9 10 19
have been observed in 81.82% of patients who underwent
Total 10 12 22 LPMR and 90.91% of patients who underwent LVMR. However,
Categorical data expressed by number of patients recurrence, impotence, and discitis were recorded as postoperative
Table 8: Functional results before and after surgery
Group A (LPMR) Group B (LVMR)
Preoperative Follow-up Preoperative Follow-up
Scoring test (Mean ± SD) (Mean ± SD) p-value (Mean ± SD) (Mean ± SD) p-value
WCS 14.28 ± 2.08 10.78 ± 2.80 0.0001 15.53 ± 2.24 6.71 ± 3.29 0.0001
BPS 3.50 ± 0.58 1.50 ± 0.58 0.003 3.60 ± 0.55 1.80 ± 0.84 0.004
ODSS 18.20 ± 1.99 6.00 ± 5.42 0.0001 18.92 ± 1.68 6.75 ± 5.06 0.0001
GIQOL 61.00 ± 8.01 105.45 ± 7.54 0.0001 66.09 ± 9.59 114.23 ± 8.64 0.0001
Categorical data expressed by mean ± standard deviation and compared by one-way ANOVA test
WCS, Wexner constipation score; BPS, Browning and Parks’ scale; ODSS, obstructed defecation syndrome score; GIQOL, gastrointestinal quality of life
scale
World Journal of Laparoscopic Surgery, Volume 15 Issue 3 (September–December 2022) 243