Page 56 - World Journal of Laparoscopic Surgery
P. 56
Laparoscopic Ventral vs Posterior Mesh Rectopexy for Rectal Prolapse
Estimated Blood Loss It was found that three patients (13.64%) in group A versus
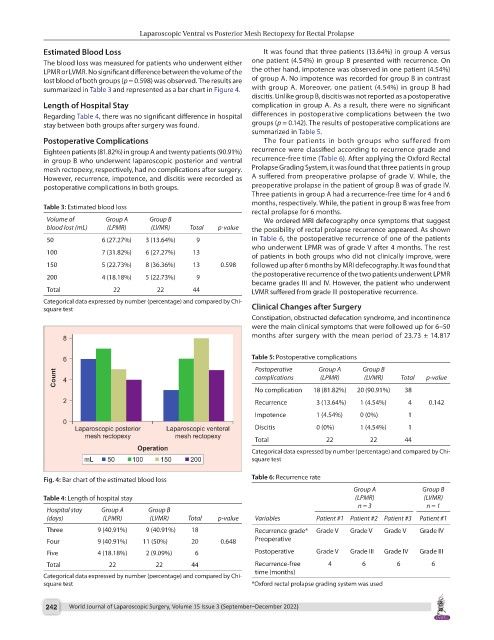
The blood loss was measured for patients who underwent either one patient (4.54%) in group B presented with recurrence. On
LPMR or LVMR. No significant difference between the volume of the the other hand, impotence was observed in one patient (4.54%)
lost blood of both groups (p = 0.598) was observed. The results are of group A. No impotence was recorded for group B in contrast
summarized in Table 3 and represented as a bar chart in Figure 4. with group A. Moreover, one patient (4.54%) in group B had
discitis. Unlike group B, discitis was not reported as a postoperative
Length of Hospital Stay complication in group A. As a result, there were no significant
Regarding Table 4, there was no significant difference in hospital differences in postoperative complications between the two
stay between both groups after surgery was found. groups (p = 0.142). The results of postoperative complications are
summarized in Table 5.
Postoperative Complications The four patients in both groups who suffered from
Eighteen patients (81.82%) in group A and twenty patients (90.91%) recurrence were classified according to recurrence grade and
in group B who underwent laparoscopic posterior and ventral recurrence-free time (Table 6). After applying the Oxford Rectal
mesh rectopexy, respectively, had no complications after surgery. Prolapse Grading System, it was found that three patients in group
However, recurrence, impotence, and discitis were recorded as A suffered from preoperative prolapse of grade V. While, the
postoperative complications in both groups. preoperative prolapse in the patient of group B was of grade IV.
Three patients in group A had a recurrence-free time for 4 and 6
months, respectively. While, the patient in group B was free from
Table 3: Estimated blood loss
rectal prolapse for 6 months.
Volume of Group A Group B We ordered MRI defecography once symptoms that suggest
blood lost (mL) (LPMR) (LVMR) Total p-value the possibility of rectal prolapse recurrence appeared. As shown
50 6 (27.27%) 3 (13.64%) 9 in Table 6, the postoperative recurrence of one of the patients
who underwent LPMR was of grade V after 4 months. The rest
100 7 (31.82%) 6 (27.27%) 13
of patients in both groups who did not clinically improve, were
150 5 (22.73%) 8 (36.36%) 13 0.598 followed up after 6 months by MRI defecography. It was found that
the postoperative recurrence of the two patients underwent LPMR
200 4 (18.18%) 5 (22.73%) 9
became grades III and IV. However, the patient who underwent
Total 22 22 44 LVMR suffered from grade III postoperative recurrence.
Categorical data expressed by number (percentage) and compared by Chi-
square test Clinical Changes after Surgery
Constipation, obstructed defecation syndrome, and incontinence
were the main clinical symptoms that were followed up for 6–50
months after surgery with the mean period of 23.73 ± 14.817
Table 5: Postoperative complications
Postoperative Group A Group B
complications (LPMR) (LVMR) Total p-value
No complication 18 (81.82%) 20 (90.91%) 38
Recurrence 3 (13.64%) 1 (4.54%) 4 0.142
Impotence 1 (4.54%) 0 (0%) 1
Discitis 0 (0%) 1 (4.54%) 1
Total 22 22 44
Categorical data expressed by number (percentage) and compared by Chi-
square test
Fig. 4: Bar chart of the estimated blood loss Table 6: Recurrence rate
Group A Group B
Table 4: Length of hospital stay (LPMR) (LVMR)
n = 3 n = 1
Hospital stay Group A Group B
(days) (LPMR) (LVMR) Total p-value Variables Patient #1 Patient #2 Patient #3 Patient #1
Three 9 (40.91%) 9 (40.91%) 18 Recurrence grade* Grade V Grade V Grade V Grade IV
Four 9 (40.91%) 11 (50%) 20 0.648 Preoperative
Five 4 (18.18%) 2 (9.09%) 6 Postoperative Grade V Grade III Grade IV Grade III
Total 22 22 44 Recurrence-free 4 6 6 6
time (months)
Categorical data expressed by number (percentage) and compared by Chi-
square test *Oxford rectal prolapse grading system was used
242 World Journal of Laparoscopic Surgery, Volume 15 Issue 3 (September–December 2022)