Page 90 - World Journal of Laparoscopic Surgery
P. 90
Elective Cholecystectomy during COVID-19
performed, as results from tests arranged in the community were not be contacted postoperatively. Demographic and treatment
not always accessible. They were also asked if they had been treated details are listed in Table 1. Fifty-one patients were of White British
for any postoperative complications. ethnicity. All patients underwent preoperative COVID-19 swab tests.
The primary outcome measure was COVID-19 related morbidity. Eight patients required a postoperative COVID-19 swab test, all of
Secondary outcome measures were non-COVID-19 related whom had a negative result. Only one patient was swabbed due to
15
morbidity as defined by the Clavien-Dindo classification, 30-day potential COVID-19 symptoms. Six patients were tested routinely
mortality, and length of hospital stay. as they were readmitted to the hospital. One patient was routinely
Only patients from the urgent waiting list were operated swabbed by their employer. One asymptomatic patient had a
on electively during this period. These include patients with positive COVID-19 swab preoperatively, they were contacted and
cholecystitis, cholangitis, pancreatitis, or recurrent severe biliary their surgery was postponed.
colic. No changes to our “urgent” classification were made during this Outcomes are detailed in Table 2. There was no COVID-19
period. Both day-case and inpatient procedures were performed. related morbidity. Of the six patients (11%) who were readmitted
Operations were performed by a consultant or supervised trainee. within 30 days of discharge, four were treated for postoperative
pain and had normal investigations, including a magnetic resonance
coVId-19 PrecAutIons And deVIAtIons cholangiopancreatogram (MRCP). One patient was readmitted with
froM the stAndArd of cAre pancreatitis which was managed conservatively following a normal
MRCP. One patient was readmitted with an occult trocar injury to the
Patient Selection small bowel and underwent two emergency laparotomies during
Patients were booked from the urgent waiting list in our usual their stay including a small bowel resection and ileostomy. Two
manner.
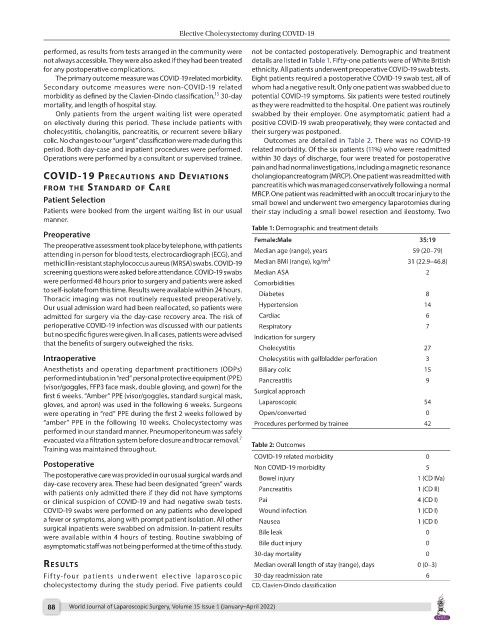
Table 1: Demographic and treatment details
Preoperative Female:Male 35:19
The preoperative assessment took place by telephone, with patients
attending in person for blood tests, electrocardiograph (ECG), and Median age (range), years 59 (20–79)
methicillin-resistant staphylococcus aureus (MRSA) swabs. COVID-19 Median BMI (range), kg/m 2 31 (22.9–46.8)
screening questions were asked before attendance. COVID-19 swabs Median ASA 2
were performed 48 hours prior to surgery and patients were asked Comorbidities
to self-isolate from this time. Results were available within 24 hours. Diabetes 8
Thoracic imaging was not routinely requested preoperatively.
Our usual admission ward had been reallocated, so patients were Hypertension 14
admitted for surgery via the day-case recovery area. The risk of Cardiac 6
perioperative COVID-19 infection was discussed with our patients Respiratory 7
but no specific figures were given. In all cases, patients were advised Indication for surgery
that the benefits of surgery outweighed the risks.
Cholecystitis 27
Intraoperative Cholecystitis with gallbladder perforation 3
Anesthetists and operating department practitioners (ODPs) Biliary colic 15
performed intubation in “red” personal protective equipment (PPE) Pancreatitis 9
(visor/goggles, FFP3 face mask, double gloving, and gown) for the
first 6 weeks. “Amber” PPE (visor/goggles, standard surgical mask, Surgical approach
gloves, and apron) was used in the following 6 weeks. Surgeons Laparoscopic 54
were operating in “red” PPE during the first 2 weeks followed by Open/converted 0
“amber” PPE in the following 10 weeks. Cholecystectomy was Procedures performed by trainee 42
performed in our standard manner. Pneumoperitoneum was safely
7
evacuated via a filtration system before closure and trocar removal.
Training was maintained throughout. Table 2: Outcomes
COVID-19 related morbidity 0
Postoperative Non COVID-19 morbidity 5
The postoperative care was provided in our usual surgical wards and Bowel injury 1 (CD IVa)
day-case recovery area. These had been designated “green” wards
with patients only admitted there if they did not have symptoms Pancreatitis 1 (CD II)
or clinical suspicion of COVID-19 and had negative swab tests. Pai 4 (CD I)
COVID-19 swabs were performed on any patients who developed Wound infection 1 (CD I)
a fever or symptoms, along with prompt patient isolation. All other Nausea 1 (CD I)
surgical inpatients were swabbed on admission. In-patient results Bile leak 0
were available within 4 hours of testing. Routine swabbing of
asymptomatic staff was not being performed at the time of this study. Bile duct injury 0
30-day mortality 0
results Median overall length of stay (range), days 0 (0–3)
Fifty-four patients underwent elective laparoscopic 30-day readmission rate 6
cholecystectomy during the study period. Five patients could CD, Clavien-Dindo classification
88 World Journal of Laparoscopic Surgery, Volume 15 Issue 1 (January–April 2022)