Page 57 - World Journal of Laparoscopic Surgery
P. 57
No External Funding Sources of Support for the Publication of Work or Study
with appendicitis and visited the hospital in the study period were 8–85.1 years with a mean age of 35 ± 15.15 years. In the OA group,
included in this study. Patients who were presented with other the mean age was 38.5 ± 17.12 years. No significant difference was
chronic illnesses and required intensive care, pregnant women, reported in the mean age of the participants (p = 0.12). Similarly,
and patients who were not willing were excluded from the study. no statistically significant difference was reported in the number
At the beginning of the study, patients were informed about the of male and female participants (p = 0.453).
study procedure and informed consent was signed. The patients No significant difference was reported in terms of co-morbidities
were also informed about both the procedures and the risk and also. The most common comorbidity reported in both the group
benefits associated with them. was hypertension followed by COPD. The total WBC count also
After the patients were confirmed they were randomly divided showed a significant difference in both the groups (p = 0.16).
into two groups, the OA group and the LA group. Each patient was The only significant difference that was observed in LA and
assigned computer-generated numbers for treatment purposes. OA group was in CRP count. In the OA group, the CRP count was
All the demographic data were collected using a special data significantly higher compared to the LA group (p = 0.024).
format. Among the study participants, 84.1% of the patients in the LA
group had uncomplicated acute appendicitis, while only 61.5% in
Surgical Procedure and Postoperative Procedure the OA group had the same. Gangrenous appendicitis was reported
The operations were performed under general anesthesia under the in 4.76% of the cases in the LA group and 9.23% of the patients in
guidance of consultant experienced surgeons. All these surgeons the OA group (Table 2).
were experienced enough to perform both the procedures and
were unknown to the data-collecting procedure. For laparoscopic Clinical Outcome and Postoperative Complications
technique, a standardized 3-port technique was used that uses Table 3 describes the outcome parameter of the LA and OA
the open (Hasson) method for establishing pneumoperitoneum. procedures. The mean operating time was almost comparable
Electrocautery was used for dissection of the mesoappendix. The between the LA and OA group. In the OA group, the operating
base of the appendix was tied and then it was divided between two time was 64 minutes and when compared to the LA group it
endo-loops with laparoscopic scissors. The specimen was retrieved was 61.5 minutes. Further analysis revealed no such statistically
inside the extraction bag. significant difference in the operating time. Blood loss was higher
Open appendectomy was performed in the standard fashion. in the OA group and the difference was statistically significant
After the ligation of the mesoappendix, the appendix was divided at (p = 0.038). Even hospital stay was also shown to be statistically
the base followed by its removal without performing invagination. higher in the OA group (average 7 days).
All the specimens were sent for microscopic examination. All the Patients who had undergone OA took more time to get back to
patients received an antibiotic regimen. In case of any technical their normal activities (15 ± 3.1). On the other hand, patients who
difficulty, laparoscopic surgeries were converted into OA. underwent LA tool-less time to resume normal activity (12 ± 2.3).
In the postoperative period, bowel sounds were monitored
every 12 hours, and once the sound was clear, the patients were Table 1: The characteristics of the patients before surgery according
put on a liquid diet. After the liquid diet was tolerated, patients to the procedure
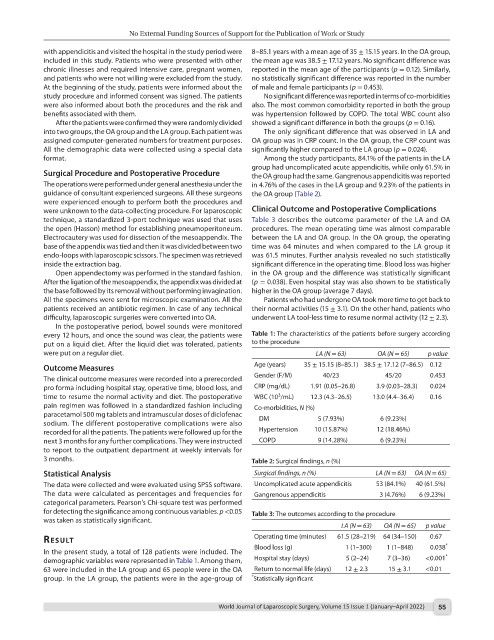
were put on a regular diet. LA (N = 63) OA (N = 65) p value
Outcome Measures Age (years) 35 ± 15.15 (8–85.1) 38.5 ± 17.12 (7–86.5) 0.12
The clinical outcome measures were recorded into a prerecorded Gender (F/M) 40/23 45/20 0.453
pro forma including hospital stay, operative time, blood loss, and CRP (mg/dL) 1.91 (0.05–26.8) 3.9 (0.03–28.3) 0.024
3
time to resume the normal activity and diet. The postoperative WBC (10 /mL) 12.3 (4.3–26.5) 13.0 (4.4–36.4) 0.16
pain regimen was followed in a standardized fashion including Co-morbidities, N (%)
paracetamol 500 mg tablets and intramuscular doses of diclofenac
sodium. The different postoperative complications were also DM 5 (7.93%) 6 (9.23%)
recorded for all the patients. The patients were followed up for the Hypertension 10 (15.87%) 12 (18.46%)
next 3 months for any further complications. They were instructed COPD 9 (14.28%) 6 (9.23%)
to report to the outpatient department at weekly intervals for
3 months. Table 2: Surgical findings, n (%)
Statistical Analysis Surgical findings, n (%) LA (N = 63) OA (N = 65)
The data were collected and were evaluated using SPSS software. Uncomplicated acute appendicitis 53 (84.1%) 40 (61.5%)
The data were calculated as percentages and frequencies for Gangrenous appendicitis 3 (4.76%) 6 (9.23%)
categorical parameters. Pearson’s Chi-square test was performed
for detecting the significance among continuous variables. p <0.05 Table 3: The outcomes according to the procedure
was taken as statistically significant.
LA (N = 63) OA (N = 65) p value
result Operating time (minutes) 61.5 (28–219) 64 (34–150) 0.67 *
In the present study, a total of 128 patients were included. The Blood loss (g) 1 (1–300) 1 (1–848) 0.038
demographic variables were represented in Table 1. Among them, Hospital stay (days) 5 (2–24) 7 (3–36) <0.001 *
63 were included in the LA group and 65 people were in the OA Return to normal life (days) 12 ± 2.3 15 ± 3.1 <0.01
group. In the LA group, the patients were in the age-group of * Statistically significant
World Journal of Laparoscopic Surgery, Volume 15 Issue 1 (January–April 2022) 55