Page 54 - World Journal of Laparoscopic Surgery
P. 54
Conversion to a Banded Gastric Bypass
Table 2: Change in weight loss metrics from nadir weight to 3-year follow-up after BGBP conversion
Nadir WT Revision 1st year P/O 2nd year P/O 3rd year P/O
WT 92.4 ± 16.1 100.5 ± 14.9 85.5 ± 10.5 82.5 ± 9.7 85.9 ± 7.1
BMI 32.5 ± 4.3 35.7 ± 4.3 29.9 ± 3.8 30.1 ± 3.8 31.3 ± 4.2
%TWL 18.5 ± 12.2 13.5 ± 10.3 25.9 ± 10.1 29.7 ± 9.2 26.9 ± 9.6
%EWL 46.4 ± 14.3 28.6 ± 11.4 61.5 ± 10.3 68.1 ± 9.4 60.6 ± 9.2
WT, weight; BMI, body mass index; %EWL, percentage of excess weight loss; %TWL, percentage of total weight loss
of which are silastic rings that may be inserted around the pouch,
proximal to the anastomosis, and are either (laparoscopically)
convertible (MiniMizer®) or nonconvertible (GaBP Ring™). Other
materials, such as linea alba, fascia lata, porcine, meshes, and
bovine grafts, have been developed; nonetheless, surgeons favor
14
silastic rings. It has been reported that a silicone band forms a
pseudocapsule, which leads to less adhesion and is simpler
to remove than other materials, but other meshes have been
demonstrated to cause scar tissue and are harder to remove. 15
We believe that dilatation of the proximal jejunum, distal to the
gastroenterostomy, plays a significant role in the creation of the neo-
stomach, leading to a complete loss of restriction. The stomach pouch
becomes more flexible over a period of time, and (all) stomas dilate.
As a result, all unsuccessful SG conversions have been addressed by
converting them to bypass procedures and placing a band across
the RYGB’s small gastric pouch. This has the effect of restricting and
starvation in the patients, resulting in successful weight loss.
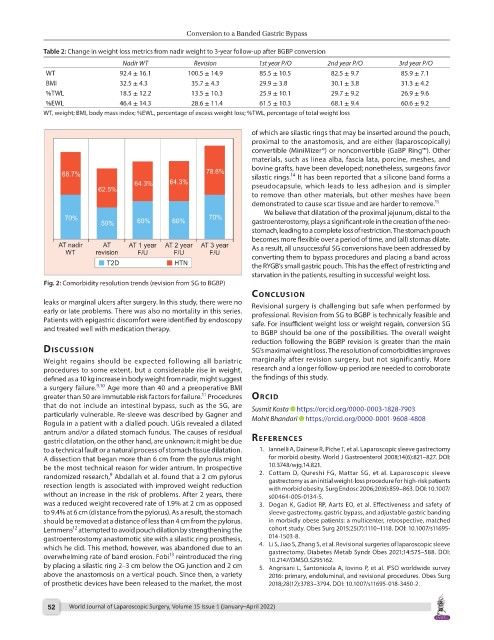
Fig. 2: Comorbidity resolution trends (revision from SG to BGBP)
conclusIon
leaks or marginal ulcers after surgery. In this study, there were no Revisional surgery is challenging but safe when performed by
early or late problems. There was also no mortality in this series. professional. Revision from SG to BGBP is technically feasible and
Patients with epigastric discomfort were identified by endoscopy safe. For insufficient weight loss or weight regain, conversion SG
and treated well with medication therapy.
to BGBP should be one of the possibilities. The overall weight
reduction following the BGBP revision is greater than the main
dIscussIon SG’s maximal weight loss. The resolution of comorbidities improves
Weight regains should be expected following all bariatric marginally after revision surgery, but not significantly. More
procedures to some extent, but a considerable rise in weight, research and a longer follow-up period are needed to corroborate
defined as a 10 kg increase in body weight from nadir, might suggest the findings of this study.
a surgery failure. 9,10 Age more than 40 and a preoperative BMI
11
greater than 50 are immutable risk factors for failure. Procedures orcId
that do not include an intestinal bypass, such as the SG, are Susmit Kosta https://orcid.org/0000-0003-1828-7903
particularly vulnerable. Re-sleeve was described by Gagner and
Rogula in a patient with a dialled pouch. UGIs revealed a dilated Mohit Bhandari https://orcid.org/0000-0001-9608-4808
antrum and/or a dilated stomach fundus. The causes of residual
gastric dilatation, on the other hand, are unknown; it might be due references
to a technical fault or a natural process of stomach tissue dilatation. 1. Iannelli A, Dainese R, Piche T, et al. Laparoscopic sleeve gastrectomy
A dissection that began more than 6 cm from the pylorus might for morbid obesity. World J Gastroenterol 2008;14(6):821–827. DOI:
be the most technical reason for wider antrum. In prospective 10.3748/wjg.14.821.
9
randomized research, Abdallah et al. found that a 2 cm pylorus 2. Cottam D, Qureshi FG, Mattar SG, et al. Laparoscopic sleeve
resection length is associated with improved weight reduction gastrectomy as an initial weight-loss procedure for high-risk patients
with morbid obesity. Surg Endosc 2006;20(6):859–863. DOI: 10.1007/
without an increase in the risk of problems. After 2 years, there s00464-005-0134-5.
was a reduced weight recovered rate of 1.9% at 2 cm as opposed 3. Dogan K, Gadiot RP, Aarts EO, et al. Effectiveness and safety of
to 9.4% at 6 cm (distance from the pylorus). As a result, the stomach sleeve gastrectomy, gastric bypass, and adjustable gastric banding
should be removed at a distance of less than 4 cm from the pylorus. in morbidly obese patients: a multicenter, retrospective, matched
12
Lemmens attempted to avoid pouch dilation by strengthening the cohort study. Obes Surg 2015;25(7):1110–1118. DOI: 10.1007/s11695-
gastroenterostomy anastomotic site with a silastic ring prosthesis, 014-1503-8.
which he did. This method, however, was abandoned due to an 4. Li S, Jiao S, Zhang S, et al. Revisional surgeries of laparoscopic sleeve
13
overwhelming rate of band erosion. Fobi reintroduced the ring gastrectomy. Diabetes Metab Syndr Obes 2021;14:575–588. DOI:
10.2147/DMSO.S295162.
by placing a silastic ring 2–3 cm below the OG junction and 2 cm 5. Angrisani L, Santonicola A, Iovino P, et al. IFSO worldwide survey
above the anastomosis on a vertical pouch. Since then, a variety 2016: primary, endoluminal, and revisional procedures. Obes Surg
of prosthetic devices have been released to the market, the most 2018;28(12):3783–3794. DOI: 10.1007/s11695-018-3450-2.
52 World Journal of Laparoscopic Surgery, Volume 15 Issue 1 (January–April 2022)