Page 53 - World Journal of Laparoscopic Surgery
P. 53
Conversion to a Banded Gastric Bypass
Sleeve Gastrectomy (range 7–60). Follow-up rate was 70.2% after the revision at 1, 2,
Veress needle is used to get access to the abdomen. The optics and 3 years, for patients eligible for a 3-year follow-up after BGBP.
are implanted through a 12 mm supra umbilical port. In the Mean patient age was 43.2 ± 12.8 years and 32 (51.6%) were
midclavicular line, a second 12 mm port is put under vision in female. Before the SG, the average starting weight in this study
2
line with the optical port. In the midclavicular line, two 5 mm was 113.5 ± 20.5 kg and the BMI 41.71 ± 8.1 kg/m . Thirteen (20.9%)
ports are inserted in the right and left subcostal regions. The had Type II diabetes mellitus (T2D), 21 (33.8%) hypertension (HTN),
liver is retracted using a Nathanson liver retractor. Transecting and 10 (16.12%) sleep apnea (SA) (Table 1). At the nadir, the average
the omentum along the larger curvature away from the stomach, weight was 92.4 ± 16.1 kg and at revision was 100.5 ± 14.9 kg. After
commencing at a location 2–3 cm from the pylorus up to the gastro conversion, the average additional weight loss was 15.02.6 kg,
esophageal junction, exposing the left crus, is how a laparoscopic which was statistically significant (p = 0.001). The mean weight after
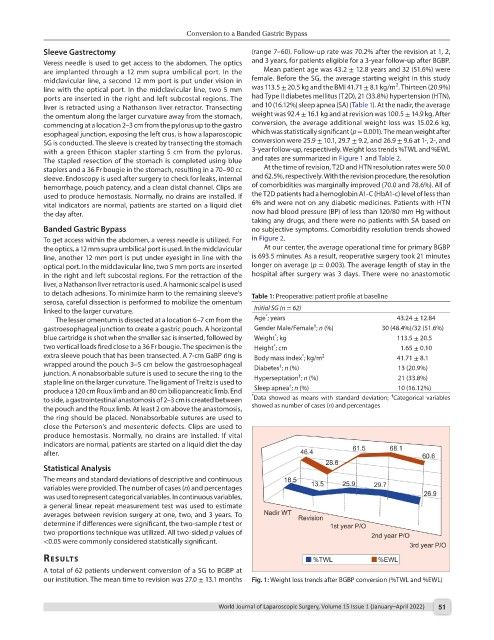
SG is conducted. The sleeve is created by transecting the stomach conversion were 25.9 ± 10.1, 29.7 ± 9.2, and 26.9 ± 9.6 at 1-, 2-, and
with a green Ethicon stapler starting 5 cm from the pylorus. 3-year follow-up, respectively. Weight loss trends %TWL and %EWL
The stapled resection of the stomach is completed using blue and rates are summarized in Figure 1 and Table 2.
staplers and a 36 Fr bougie in the stomach, resulting in a 70–90 cc At the time of revision, T2D and HTN resolution rates were 50.0
sleeve. Endoscopy is used after surgery to check for leaks, internal and 62.5%, respectively. With the revision procedure, the resolution
hemorrhage, pouch patency, and a clean distal channel. Clips are of comorbidities was marginally improved (70.0 and 78.6%). All of
used to produce hemostasis. Normally, no drains are installed. If the T2D patients had a hemoglobin A1-C (HbA1-c) level of less than
vital indicators are normal, patients are started on a liquid diet 6% and were not on any diabetic medicines. Patients with HTN
the day after. now had blood pressure (BP) of less than 120/80 mm Hg without
taking any drugs, and there were no patients with SA based on
Banded Gastric Bypass no subjective symptoms. Comorbidity resolution trends showed
To get access within the abdomen, a veress needle is utilized. For in Figure 2.
the optics, a 12 mm supra umbilical port is used. In the midclavicular At our center, the average operational time for primary BGBP
line, another 12 mm port is put under eyesight in line with the is 693.5 minutes. As a result, reoperative surgery took 21 minutes
optical port. In the midclavicular line, two 5 mm ports are inserted longer on average (p = 0.003). The average length of stay in the
in the right and left subcostal regions. For the retraction of the hospital after surgery was 3 days. There were no anastomotic
liver, a Nathanson liver retractor is used. A harmonic scalpel is used
to detach adhesions. To minimize harm to the remaining sleeve’s Table 1: Preoperative: patient profile at baseline
serosa, careful dissection is performed to mobilize the omentum
linked to the larger curvature. Initial SG (n = 62)
*
The lesser omentum is dissected at a location 6–7 cm from the Age ; years 43.24 ± 12.84
†
gastroesophageal junction to create a gastric pouch. A horizontal Gender Male/Female ; n (%) 30 (48.4%)/32 (51.6%)
blue cartridge is shot when the smaller sac is inserted, followed by Weight ; kg 113.5 ± 20.5
*
two vertical loads fired close to a 36 Fr bougie. The specimen is the Height ; cm 1.65 ± 0.10
*
extra sleeve pouch that has been transected. A 7-cm GaBP ring is Body mass index ; kg/m 2 41.71 ± 8.1
*
wrapped around the pouch 3–5 cm below the gastroesophageal Diabetes ; n (%) 13 (20.9%)
†
junction. A nonabsorbable suture is used to secure the ring to the †
staple line on the larger curvature. The ligament of Treitz is used to Hyperseptation ; n (%) 21 (33.8%)
†
produce a 120 cm Roux limb and an 80 cm biliopancreatic limb. End Sleep apnea ; n (%) 10 (16.12%)
†
to side, a gastrointestinal anastomosis of 2–3 cm is created between * Data showed as means with standard deviation; Categorical variables
the pouch and the Roux limb. At least 2 cm above the anastomosis, showed as number of cases (n) and percentages
the ring should be placed. Nonabsorbable sutures are used to
close the Peterson’s and mesenteric defects. Clips are used to
produce hemostasis. Normally, no drains are installed. If vital
indicators are normal, patients are started on a liquid diet the day
after.
Statistical Analysis
The means and standard deviations of descriptive and continuous
variables were provided. The number of cases (n) and percentages
was used to represent categorical variables. In continuous variables,
a general linear repeat measurement test was used to estimate
averages between revision surgery at one, two, and 3 years. To
determine if differences were significant, the two-sample t test or
two-proportions technique was utilized. All two-sided p values of
<0.05 were commonly considered statistically significant.
results
A total of 62 patients underwent conversion of a SG to BGBP at
our institution. The mean time to revision was 27.0 ± 13.1 months Fig. 1: Weight loss trends after BGBP conversion (%TWL and %EWL)
World Journal of Laparoscopic Surgery, Volume 15 Issue 1 (January–April 2022) 51