Page 10 - tmp
P. 10
Laparoscopic Cholecystectomy for Acute Cholecystitis
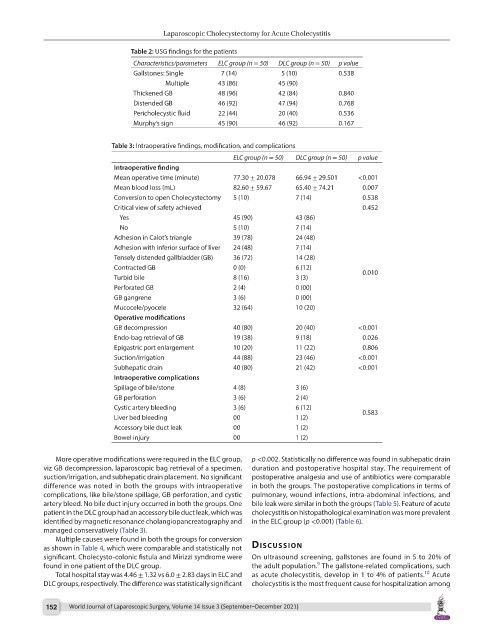
Table 2: USG findings for the patients
Characteristics/parameters ELC group (n = 50) DLC group (n = 50) p value
Gallstones: Single 7 (14) 5 (10) 0.538
Multiple 43 (86) 45 (90)
Thickened GB 48 (96) 42 (84) 0.840
Distended GB 46 (92) 47 (94) 0.768
Pericholecystic fluid 22 (44) 20 (40) 0.536
Murphy’s sign 45 (90) 46 (92) 0.167
Table 3: Intraoperative findings, modification, and complications
ELC group (n = 50) DLC group (n = 50) p value
Intraoperative finding
Mean operative time (minute) 77.30 ± 20.078 66.94 ± 29.501 <0.001
Mean blood loss (mL) 82.60 ± 59.67 65.40 ± 74.21 0.007
Conversion to open Cholecystectomy 5 (10) 7 (14) 0.538
Critical view of safety achieved 0.452
Yes 45 (90) 43 (86)
No 5 (10) 7 (14)
Adhesion in Calot’s triangle 39 (78) 24 (48)
Adhesion with inferior surface of liver 24 (48) 7 (14)
Tensely distended gallbladder (GB) 36 (72) 14 (28)
Contracted GB 0 (0) 6 (12) 0.010
Turbid bile 8 (16) 3 (3)
Perforated GB 2 (4) 0 (00)
GB gangrene 3 (6) 0 (00)
Mucocele/pyocele 32 (64) 10 (20)
Operative modifications
GB decompression 40 (80) 20 (40) <0.001
Endo-bag retrieval of GB 19 (38) 9 (18) 0.026
Epigastric port enlargement 10 (20) 11 (22) 0.806
Suction/irrigation 44 (88) 23 (46) <0.001
Subhepatic drain 40 (80) 21 (42) <0.001
Intraoperative complications
Spillage of bile/stone 4 (8) 3 (6)
GB perforation 3 (6) 2 (4)
Cystic artery bleeding 3 (6) 6 (12) 0.583
Liver bed bleeding 00 1 (2)
Accessory bile duct leak 00 1 (2)
Bowel injury 00 1 (2)
More operative modifications were required in the ELC group, p <0.002. Statistically no difference was found in subhepatic drain
viz GB decompression, laparoscopic bag retrieval of a specimen, duration and postoperative hospital stay. The requirement of
suction/irrigation, and subhepatic drain placement. No significant postoperative analgesia and use of antibiotics were comparable
difference was noted in both the groups with intraoperative in both the groups. The postoperative complications in terms of
complications, like bile/stone spillage, GB perforation, and cystic pulmonary, wound infections, intra-abdominal infections, and
artery bleed. No bile duct injury occurred in both the groups. One bile leak were similar in both the groups (Table 5). Feature of acute
patient in the DLC group had an accessory bile duct leak, which was cholecystitis on histopathological examination was more prevalent
identified by magnetic resonance cholangiopancreatography and in the ELC group (p <0.001) (Table 6).
managed conservatively (Table 3).
Multiple causes were found in both the groups for conversion
as shown in Table 4, which were comparable and statistically not dIscussIon
significant. Cholecysto-colonic fistula and Mirizzi syndrome were On ultrasound screening, gallstones are found in 5 to 20% of
9
found in one patient of the DLC group. the adult population. The gallstone-related complications, such
10
Total hospital stay was 4.46 ± 1.32 vs 6.0 ± 2.83 days in ELC and as acute cholecystitis, develop in 1 to 4% of patients. Acute
DLC groups, respectively. The difference was statistically significant cholecystitis is the most frequent cause for hospitalization among
152 World Journal of Laparoscopic Surgery, Volume 14 Issue 3 (September–December 2021)