Page 11 - tmp
P. 11
Laparoscopic Cholecystectomy for Acute Cholecystitis
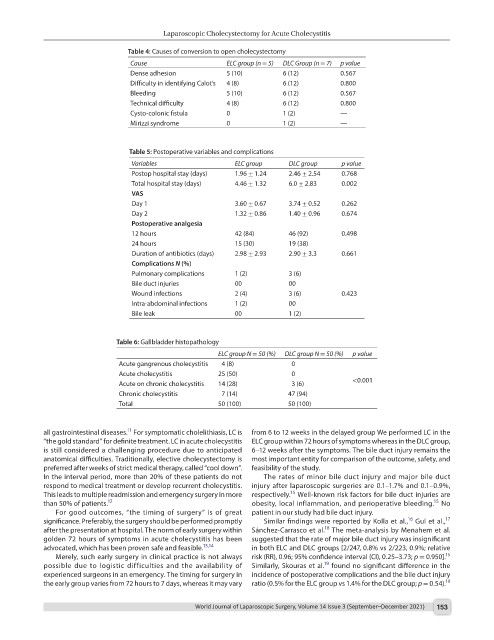
Table 4: Causes of conversion to open cholecystectomy
Cause ELC group (n = 5) DLC Group (n = 7) p value
Dense adhesion 5 (10) 6 (12) 0.567
Difficulty in identifying Calot’s 4 (8) 6 (12) 0.800
Bleeding 5 (10) 6 (12) 0.567
Technical difficulty 4 (8) 6 (12) 0.800
Cysto-colonic fistula 0 1 (2) —
Mirizzi syndrome 0 1 (2) —
Table 5: Postoperative variables and complications
Variables ELC group DLC group p value
Postop hospital stay (days) 1.96 ± 1.24 2.46 ± 2.54 0.768
Total hospital stay (days) 4.46 ± 1.32 6.0 ± 2.83 0.002
VAS
Day 1 3.60 ± 0.67 3.74 ± 0.52 0.262
Day 2 1.32 ± 0.86 1.40 ± 0.96 0.674
Postoperative analgesia
12 hours 42 (84) 46 (92) 0.498
24 hours 15 (30) 19 (38)
Duration of antibiotics (days) 2.98 ± 2.93 2.90 ± 3.3 0.661
Complications N (%)
Pulmonary complications 1 (2) 3 (6)
Bile duct injuries 00 00
Wound infections 2 (4) 3 (6) 0.423
Intra-abdominal infections 1 (2) 00
Bile leak 00 1 (2)
Table 6: Gallbladder histopathology
ELC group N = 50 (%) DLC group N = 50 (%) p value
Acute gangrenous cholecystitis 4 (8) 0
Acute cholecystitis 25 (50) 0
Acute on chronic cholecystitis 14 (28) 3 (6) <0.001
Chronic cholecystitis 7 (14) 47 (94)
Total 50 (100) 50 (100)
11
all gastrointestinal diseases. For symptomatic cholelithiasis, LC is from 6 to 12 weeks in the delayed group We performed LC in the
“the gold standard” for definite treatment. LC in acute cholecystitis ELC group within 72 hours of symptoms whereas in the DLC group,
is still considered a challenging procedure due to anticipated 6–12 weeks after the symptoms. The bile duct injury remains the
anatomical difficulties. Traditionally, elective cholecystectomy is most important entity for comparison of the outcome, safety, and
preferred after weeks of strict medical therapy, called “cool down”. feasibility of the study.
In the interval period, more than 20% of these patients do not The rates of minor bile duct injury and major bile duct
respond to medical treatment or develop recurrent cholecystitis. injury after laparoscopic surgeries are 0.1–1.7% and 0.1–0.9%,
15
This leads to multiple readmission and emergency surgery in more respectively. Well-known risk factors for bile duct injuries are
15
than 50% of patients. 12 obesity, local inflammation, and perioperative bleeding. No
For good outcomes, “the timing of surgery” is of great patient in our study had bile duct injury.
16
17
significance. Preferably, the surgery should be performed promptly Similar findings were reported by Kolla et al., Gul et al.,
18
after the presentation at hospital. The norm of early surgery within Sánchez-Carrasco et al. The meta-analysis by Menahem et al.
golden 72 hours of symptoms in acute cholecystitis has been suggested that the rate of major bile duct injury was insignificant
advocated, which has been proven safe and feasible. 13,14 in both ELC and DLC groups [2/247, 0.8% vs 2/223, 0.9%; relative
15
Merely, such early surgery in clinical practice is not always risk (RR), 0.96; 95% confidence interval (CI), 0.25–3.73; p = 0.950].
19
possible due to logistic difficulties and the availability of Similarly, Skouras et al. found no significant difference in the
experienced surgeons in an emergency. The timing for surgery in incidence of postoperative complications and the bile duct injury
the early group varies from 72 hours to 7 days, whereas it may vary ratio (0.5% for the ELC group vs 1.4% for the DLC group; p = 0.54). 19
World Journal of Laparoscopic Surgery, Volume 14 Issue 3 (September–December 2021) 153