Page 12 - tmp
P. 12
Laparoscopic Cholecystectomy for Acute Cholecystitis
In our study, the mean blood loss was significantly more in
ELC than DLC group, because of inflammatory reactions leading
to neovascularity, adhesions around GB, and Calot's triangle in the
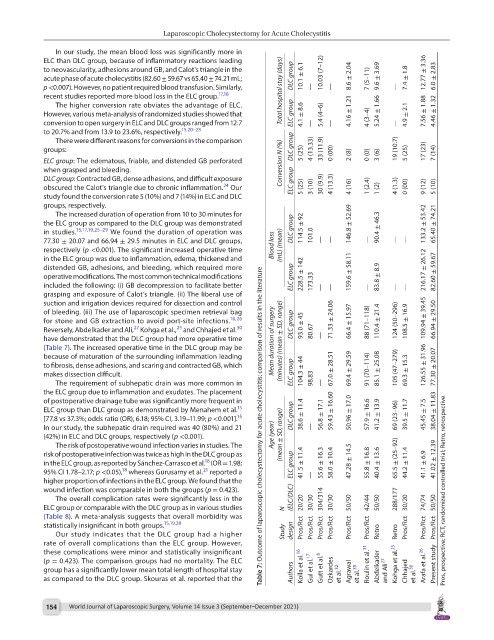
acute phase of acute cholecystitis (82.60 ± 59.67 vs 65.40 ± 74.21 mL; DLC group 10.1 ± 6.1 10.03 (7–12) 8.6 ± 2.04 7 (5–11) 9.6 ± 3.69 7.4 ± 1.8 12.77 ± 3.36 6.0 ± 2.83
p <0.007). However, no patient required blood transfusion. Similarly, — — —
recent studies reported more blood loss in the ELC group. 17,18 Total hospital stay (days)
The higher conversion rate obviates the advantage of ELC.
However, various meta-analysis of randomized studies showed that ELC group 4.1 ± 8.6 5.4 (4–6) 4.16 ± 1.21 4 (3–4) 5.24 ± 1.66 4.9 ± 2.1 7.56 ± 1.88 4.46 ± 1.32
conversion to open surgery in ELC and DLC groups ranged from 12.7 — — —
to 20.7% and from 13.9 to 23.6%, respectively. 15,20–23
There were different reasons for conversions in the comparison
groups: DLC group 5 (25) 4 (13.33) 33 (11.9) 0 (00) 19 (10.7) 5 (25) 17 (23) 7 (14)
ELC group: The edematous, friable, and distended GB perforated Conversion N (%) 2 (8) 0 (0) 3 (6)
when grasped and bleeding.
DLC group: Contracted GB, dense adhesions, and difficult exposure ELC group
24
obscured the Calot's triangle due to chronic inflammation. Our 5 (25) 3 (10) 30 (9.9) 4 (13.3) 4 (16) 1 (2.4) 1 (2) 4 (1.3) 0 (00) 9 (12) 5 (10)
study found the conversion rate 5 (10%) and 7 (14%) in ELC and DLC
groups, respectively.
The increased duration of operation from 10 to 30 minutes for
the ELC group as compared to the DLC group was demonstrated 146.8 ± 52.69 133.2 ± 53.42 65.40 ± 74.21
in studies. 15,17,19,25–29 We found the duration of operation was DLC group 114.5 ± 92 90.4 ± 46.3
77.30 ± 20.07 and 66.94 ± 29.5 minutes in ELC and DLC groups, Blood loss 101.0 — — — — —
respectively (p <0.001). The significant increased operative time (mL) (mean)
in the ELC group was due to inflammation, edema, thickened and
distended GB, adhesions, and bleeding, which required more 216.17 ± 26.12
operative modifications. The most common technical modifications ELC group 228.5 ± 142 159.6 ± 58.11 83.8 ± 8.9 82.60 ± 59.67
included the following: (i) GB decompression to facilitate better 173.33 — — — — —
grasping and exposure of Calot’s triangle. (ii) The liberal use of
suction and irrigation devices required for dissection and control
of bleeding. (iii) The use of laparoscopic specimen retrieval bag
for stone and GB extraction to avoid port-site infections. 16,26 71.33 ± 24.06 66.4 ± 15.97 88 (71–118) 110.4 ± 21.4 124 (50–296) 108.5 ± 16.9 109.94 ± 39.45 66.94 ± 29.50
30
25
27
Reversely, Abdelkader and Ali, Kohga et al., and Chhajed et al. DLC group 93.0 ± 45 80.67
have demonstrated that the DLC group had more operative time Mean duration of surgery (minutes) (mean ± SD, range) —
(Table 7). The increased operative time in the DLC group may be
because of maturation of the surrounding inflammation leading
to fibrosis, dense adhesions, and scaring and contracted GB, which 105 (47–279) 126.55 ± 31.96 77.30 ± 20.07
makes dissection difficult. ELC group 104.3 ± 44 67.0 ± 28.51 69.4 ± 29.59 91 (70–114) 85.1 ± 25.08 69.3 ± 15.3
The requirement of subhepatic drain was more common in 98.83 —
the ELC group due to inflammation and exudates. The placement
of postoperative drainage tube was significantly more frequent in
15
ELC group than DLC group as demonstrated by Menahem et al. 59.43 ± 16.60 38.04 ± 11.83
15
[77.8 vs 37.3%; odds ratio (OR), 6.18; 95% CI, 3.19–11.99; p <0.001]. DLC group 38.6 ± 11.4 56.8 ± 17.1 50.96 ± 17.0 57.9 ± 16.6 41.2 ± 13.9 69 (23–96) 39.5 ± 11.7 45.45 ± 7.5
In our study, the subhepatic drain required was 40 (80%) and 21 Table 7: Outcome of laparoscopic cholecystectomy for acute cholecystitis: comparison of results in the literature —
(42%) in ELC and DLC groups, respectively (p <0.001). Age (year) (mean ± SD, range)
The risk of postoperative wound infection varies in studies. The
risk of postoperative infection was twice as high in the DLC group as
18
in the ELC group, as reported by Sánchez-Carrasco et al. (OR = 1.98; ELC group 41.5 ± 11.4 55.6 ± 16.3 58.0 ± 10.4 47.28 ± 14.5 55.8 ± 16.8 40.4 ± 13.6 65.5 ± (25–92) 44.2 ± 11.4 41.1 ± 6.9 41.02 ± 12.39
18
21
95% CI 1.78–2.17; p <0.05), whereas Gurusamy et al. reported a
higher proportion of infections in the ELC group. We found that the —
wound infection was comparable in both the groups (p = 0.423). Pros, prospective; RCT, randomized controlled trial; Retro, retrospective
The overall complication rates were significantly less in the (ELC/DLC) 304/314 288/177
ELC group or comparable with the DLC group as in various studies N 20/20 30/30 30/30 50/50 42/44 50/50 30/20 74/74 50/50
(Table 8). A meta-analysis suggests that overall morbidity was
statistically insignificant in both groups. 15,19,28 Pros/Rct Pros/Rct Pros/Rct Pros/Rct Pros/Rct Pros/Rct Pros/Rct Pros/Rct Pros/Rct
Our study indicates that the DLC group had a higher Study design Retro Retro
rate of overall complications than the ELC group. However,
these complications were minor and statistically insignificant
(p = 0.423). The comparison groups had no mortality. The ELC
group has a significantly lower mean total length of hospital stay Kolla et al. 16 Gul et al. 17 Gutt et al. 8 Ozkardes Agrawal Roulin et al. 31 Abdelkader and Ali 27 Kohga et al. 25 Chhajed Arafa et al. 26 Present study
as compared to the DLC group. Skouras et al. reported that the Authors et al. 32 et al. 35 et al. 30
154 World Journal of Laparoscopic Surgery, Volume 14 Issue 3 (September–December 2021)