Page 12 - World Journal of Laparoscopic Surgery
P. 12
Ganeshselvi Premkumar
endometrial cells through the fallopian tubes. These cells are cyclical hematuria, cyclical dysuria, ureteric obstruction, cyclical
capable of implantation and development. Dissemination to hemoptysis, cyclical pain and swelling in the umbilicus or scars.
distant sites is possible by lymphatic and vascular spread. This
theory remains the most popular and is supported by PATHOGENESIS OF INFERTILITY IN
experiments that show that endometrial cells are viable both in ENDOMETRIOSIS
2
3
vitro and in vivo. The exact mechanism of endometrioma The nature of the relationship between endometriosis and
formation is unknown. One possibility is the formation of an infertility remains controversial. One recent study suggests that
adhesion between the ovary and pelvic peritoneum and the the presence of endometriosis alone where no other cause is
progressive infolding of the ovary forming a pseudo cyst called found affects fertility. But the mechanism by which minimal
7
an endometrioma. endometriosis affects fertility in such women is uncertain. It is
The coelomic metaplasia theory explains the unusual sites
of endometriosis but evidence for it has yet to be established. accepted that moderate-severe endometriosis is likely to result
in infertility because of adhesions disrupting the anatomical
4
Dr Meyer proposed that coelomic epithelium undergoes relationships between fallopian tube and ovary. Furthermore,
metaplasia to become endometriosis. Endometriosis does not severe dyspareunia and pelvic pain preventing regular sexual
show the distribution with older age that is found in other organs intercourse could also affect fertility.
that undergo metaplasia, e.g. squamous metaplasia in the lung.
Iatrogenic dissemination can occur during gynecological
procedures, but it is not clear whether the rate of transplantation DIAGNOSIS OF ENDOMETRIOSIS
varies with the time of cycle. Recent work on pathogenesis A clinical history of pelvic pain, particularly if related to the
showed immunogenetic defects, e.g. aberrant expression of menstrual cycle always suggests a diagnosis of endometriosis.
factor. Steroidogenic Factor-1 activates the expression of the Examination may reveal tenderness or an adnexal mass.
5
aromatase enzyme and increased expression of cyclo- Ultrasound scanning, computerized tomography scan, and
oxygenase-2 in the stromal cells. 6
magnetic resonance imaging may assist in the diagnosis, but
none are highly specific and a normal result does not exclude
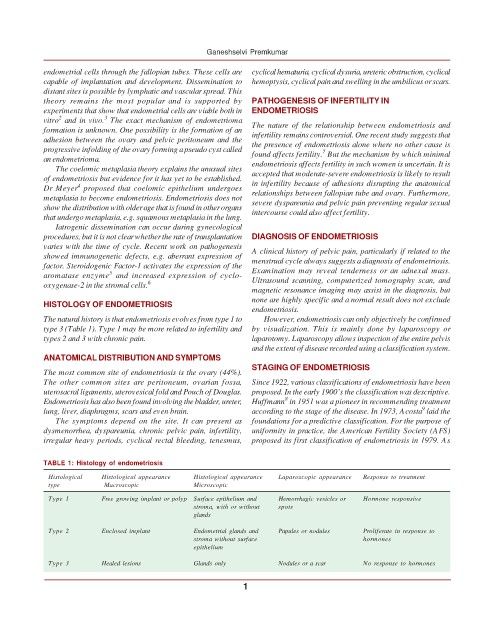
HISTOLOGY OF ENDOMETRIOSIS
endometriosis.
The natural history is that endometriosis evolves from type 1 to However, endometriosis can only objectively be confirmed
type 3 (Table 1). Type 1 may be more related to infertility and by visualization. This is mainly done by laparoscopy or
types 2 and 3 with chronic pain. laparotomy. Laparoscopy allows inspection of the entire pelvis
and the extent of disease recorded using a classification system.
ANATOMICAL DISTRIBUTION AND SYMPTOMS
STAGING OF ENDOMETRIOSIS
The most common site of endometriosis is the ovary (44%).
The other common sites are peritoneum, ovarian fossa, Since 1922, various classifications of endometriosis have been
uterosacral ligaments, uterovesical fold and Pouch of Douglas. proposed. In the early 1900’s the classification was descriptive.
8
Endometriosis has also been found involving the bladder, ureter, Huffmann in 1951 was a pioneer in recommending treatment
9
lung, liver, diaphragms, scars and even brain. according to the stage of the disease. In 1973, Acosta laid the
The symptoms depend on the site. It can present as foundations for a predictive classification. For the purpose of
dysmenorrhea, dyspareunia, chronic pelvic pain, infertility, uniformity in practice, the American Fertility Society (AFS)
irregular heavy periods, cyclical rectal bleeding, tenesmus, proposed its first classification of endometriosis in 1979. As
TABLE 1: Histology of endometriosis
Histological Histological appearance Histological appearance Laparoscopic appearance Response to treatment
type Macroscopic Microscopic
Type 1 Free growing implant or polyp Surface epithelium and Hemorrhagic vesicles or Hormone responsive
stroma, with or without spots
glands
Type 2 Enclosed implant Endometrial glands and Papules or nodules Proliferate in response to
stroma without surface hormones
epithelium
Type 3 Healed lesions Glands only Nodules or a scar No response to hormones
10