Page 13 - WJOLS
P. 13
Laparoscopic Ultrasound–Guided versus Percutaneous Radiofrequency Ablation in Treatment of Unresectable HCC
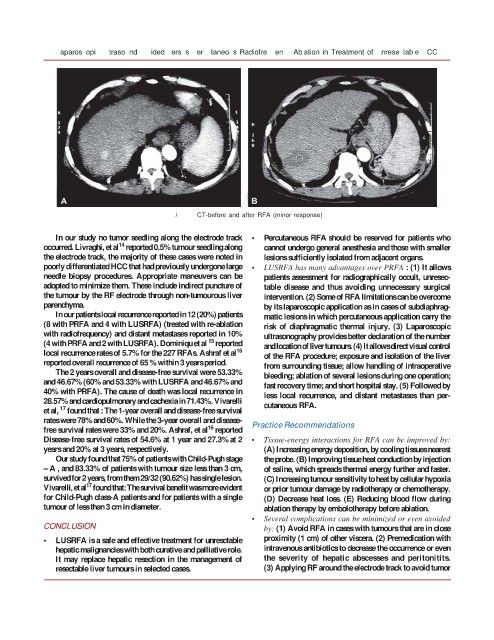
Fig. 13: CT-before and after RFA (minor response)
In our study no tumor seedling along the electrode track • Percutaneous RFA should be reserved for patients who
14
occurred. Livraghi, et al reported 0.5% tumour seedling along cannot undergo general anesthesia and those with smaller
the electrode track, the majority of these cases were noted in lesions sufficiently isolated from adjacent organs.
poorly differentiated HCC that had previously undergone large • LUSRFA has many advantages over PRFA : (1) It allows
needle biopsy procedures. Appropriate maneuvers can be patients assessment for radiographically occult, unresec-
adopted to minimize them. These include indirect puncture of table disease and thus avoiding unnecessary surgical
the tumour by the RF electrode through non-tumourous liver intervention. (2) Some of RFA limitations can be overcome
parenchyma. by its laparoscopic application as in cases of subdiaphrag-
In our patients local recurrence reported in 12 (20%) patients matic lesions in which percutaneous application carry the
(8 with PRFA and 4 with LUSRFA) (treated with re-ablation risk of diaphragmatic thermal injury. (3) Laparoscopic
with radiofrequency) and distant metastases reported in 10% ultrasonography provides better declaration of the number
15
(4 with PRFA and 2 with LUSRFA). Dominiqu et al reported and location of liver tumours. (4) It allows direct visual control
local recurrence rates of 5.7% for the 227 RFAs. Ashraf et al 16 of the RFA procedure; exposure and isolation of the liver
reported overall recurrence of 65 % within 3 years period. from surrounding tissue; allow handling of intraoperative
The 2 years overall and disease-free survival were 53.33% bleeding; ablation of several lesions during one operation;
and 46.67% (60% and 53.33% with LUSRFA and 46.67% and fast recovery time; and short hospital stay. (5) Followed by
40% with PRFA). The cause of death was local recurrence in less local recurrence, and distant metastases than per-
28.57% and cardiopulmonary and cachexia in 71.43%. Vivarelli cutaneous RFA.
17
et al, found that : The 1-year overall and disease-free survival
rates were 78% and 60%. While the 3-year overall and disease- Practice Recommendations
16
free survival rates were 33% and 20%. Ashraf, et al reported
Disease-free survival rates of 54.6% at 1 year and 27.3% at 2 • Tissue-energy interactions for RFA can be improved by:
years and 20% at 3 years, respectively. (A) Increasing energy deposition, by cooling tissues nearest
Our study found that 75% of patients with Child-Pugh stage the probe. (B) Improving tissue heat conduction by injection
– A , and 83.33% of patients with tumour size less than 3 cm, of saline, which spreads thermal energy further and faster.
survived for 2 years, from them 29/32 (90.62%) has single lesion. (C) Increasing tumour sensitivity to heat by cellular hypoxia
17
Vivarelli, et al found that: The survival benefit was more evident or prior tumour damage by radiotherapy or chemotherapy.
for Child-Pugh class-A patients and for patients with a single (D) Decrease heat loss. (E) Reducing blood flow during
tumour of less than 3 cm in diameter. ablation therapy by embolotherapy before ablation.
• Several complications can be minimized or even avoided
CONCLUSION by: (1) Avoid RFA in cases with tumours that are in close
• LUSRFA is a safe and effective treatment for unresctable proximity (1 cm) of other viscera. (2) Premedication with
hepatic malignancies with both curative and palliative role. intravenous antibiotics to decrease the occurrence or even
It may replace hepatic resection in the management of the severity of hepatic abscesses and peritonitits.
resectable liver tumours in selected cases. (3) Applying RF around the electrode track to avoid tumor
11